Regional Update
Welcome to the first AP Faculty update of 2022. As ever these first few months of the year have kept us busy and provided plenty of opportunities to showcase the great work being done in advancing practice across the region.

Scoping Update
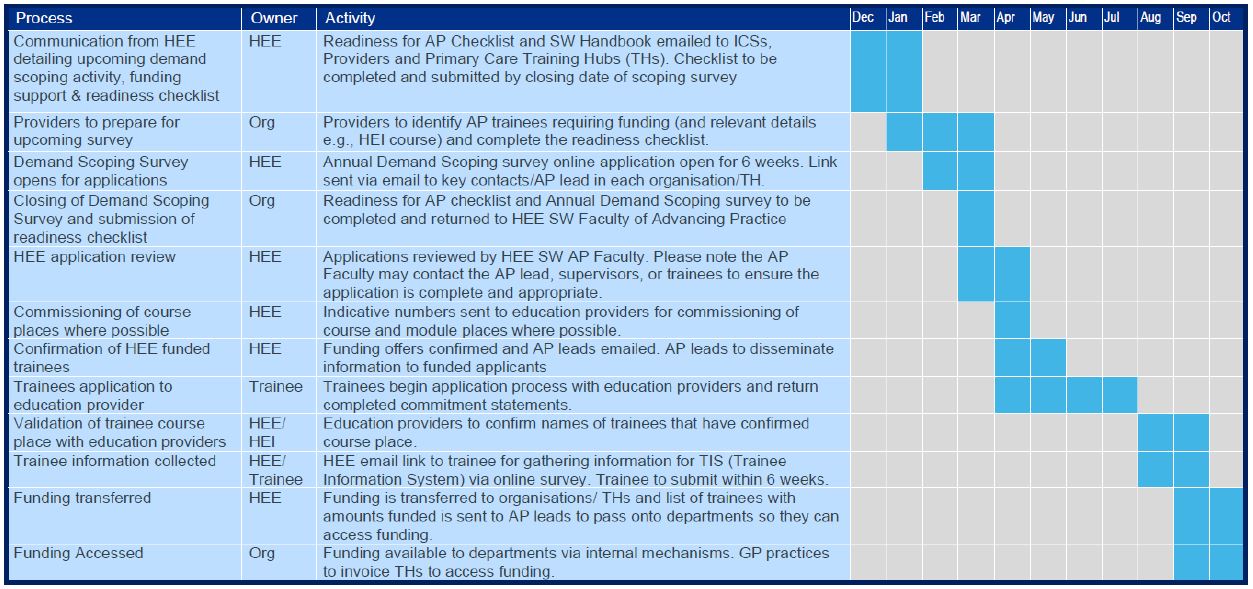
The 2022/23 Annual Demand Scoping for HEE Faculty funding of trainee Advanced Practitioners opened for 6 weeks at the start of February and closed on 15th March 2022. The Faculty team are currently reviewing all the applications that have been submitted. We want to thank all our partners across the South West for taking the time to consider and complete these applications.
The team aim to have reviewed all submissions by the end of April 2022 and we will use the results to inform discussions with education providers across the South West of potential trainee numbers for 2022/23. The aim being that wherever possible education provider are able to plan to ensure adequate capacity to support all aspiring trainees.
When the offer of funding is extended to eligible trainees, they will be required to apply for their chosen MSc Advanced Practice course. Please note funding is dependent upon their place being confirmed by the education provider. Employers, in conjunction with their trainees, will be required to complete and return commitment statements for each trainee, as a requirement to secure their funding. These next steps are laid out in more detail within our Annual Funding Timeline shown below.
For more information please refer to our handbook.
Networking Event
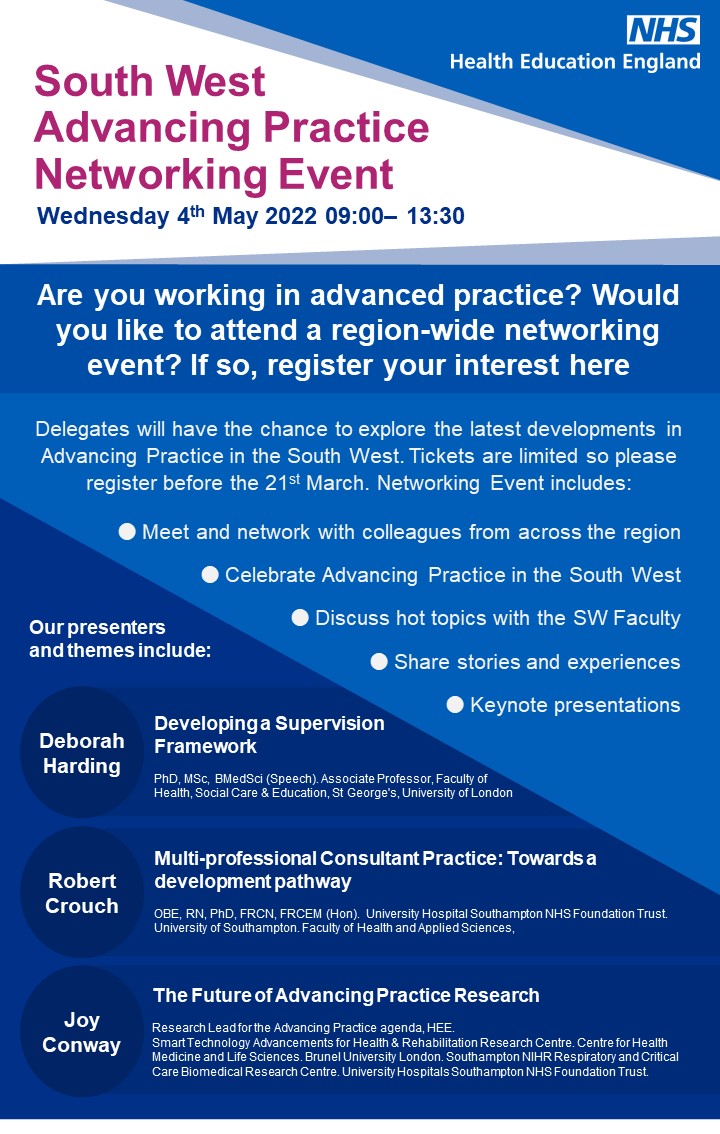
We are delighted to announce that we will be running a SW AP Networking Event on 4th May which will run from 9:00am-1:10pm and feature keynote speakers who lead the HEE CoAP developments in: supervision, research and AP careers beyond the attainment of AP MSc and HEE recognition.
The Regional team will also be sharing their own experience and our more local developments on topics relating to the trainee environment and educational supervision. There will also be the opportunity for delegates to get involved in hot topic discussions, and interact with peers from across the region.
All sessions will be recorded so if you have not signed up or were unable to secure a place as these are limited, we will be providing the recording to all registrants to the event and our mailing list. For more information about the event please click here.
We aim for this to be the first of what will become an annual event so if you don’t want to miss out on the next one, or would like to be kept informed about any other events, please sign up to our mailing list here.
South West Regional Website Refresh
The Advancing Practice website was launched back in June 2021, and for the first 6 months included a single South West regional page with a short introduction to our region and team.
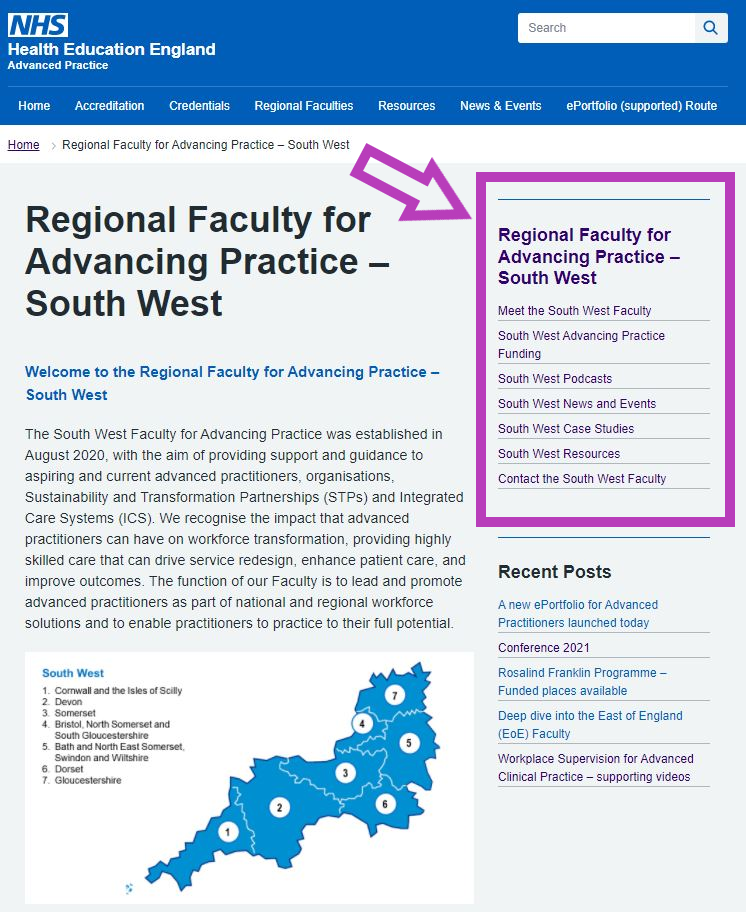
Since January the Faculty have been working on refreshing the content and restructuring the South West regional section to make it easier to navigate and more informative.
As well as an introduction to the region, our homepage now features a side bar with new pages, full of information about Advancing Practice in the South West.
- Meet the South West Faculty – Find out about the members South West Faculty and what they do.
- South West Advancing Practice Funding – Get information on this year’s funding offer for Advancing Practice in the South West, find information on how to apply and a copy of our annual funding timeline.
- South West Podcasts – Listen to our podcasts discussing a range of Advanced Practice topics and themes.
- South West News and Events – Find out about upcoming regional events and read all about what the Faculty have been up to in our quarterly news updates.
- South West Case Studies – Learn more about the trailblazing Advanced Practitioners in the region, and how they are helping to transform service delivery in order to better meet local healthcare needs.
- South West Resources – Find copies of all our South West resources, including our South West Handbook, Readiness for Advanced Practice Checklist and information and recordings from our scoping webinar.
There is new information being added regularly so please check it out here.
South West Faculty Podcast Series
At the end of November 2021, during Advancing Practice Week, the Faculty launched our new Advanced Practice Podcast series. The series is hosted by members of the South West Faculty and discusses Advancing Practice challenges, themes and topics from across the South West region.

Guests featured in the series include not only Advanced Practitioners but, Advanced Practice Leads, Experts and Consultants, as well as Trainee’s discussing their journey to qualifying as Advanced Practitioners.
This popular series now has three episodes discussing various topics in Advancing Practice.
- The first episode discusses the journey of training as an emergency care advanced practitioner. What it takes to train an EC ACP and lessons learned along the way, from the perspectives of a trainee, an AP lead, and an educational supervisor.
- The second looks at the narrative around advanced practice in relation to Allied Health Professionals. Exploring the challenges and opportunities that the AHP workforce face when training for and progressing into Advanced Practice roles.
- The third follows the journey of Advanced Neonatal Nurse Practitioners (ANNP) in relation to training, career progression and service development. It explores the experiences of ANNPs at different stages of their career, as they reflect upon how ANNP training, supervision and career opportunities have evolved, the challenges and the future of ANNP.
All our faculty podcasts can be found here and are available on most major streaming platforms. Make sure you follow @NHSHEE_SWest on twitter to find out when the next episodes are released!
Focus on Radiography
Martin Nelson (Advancing Practice Supervision & Assessment Lead for Radiography, Oncology South West Faculty of Advancing Practice Health Education England)
The recent creation of the National Centre for Advancing Practice has moved the emphasis of developing Advanced Practice (AP) from a professional monitored and driven enterprise to a centrally funded agenda that recognises, promotes and develops all registered non-medical professional groups equally.
I have recently taken a role at Health Education England as the Advancing Practice Supervision and Assessment Lead for Radiography and Oncology, and very much relish the opportunity to address some of the myths, and misconceptions around AP in radiography, to explain what HEE is hoping to achieve, the funding available, how this can be achieved but also to be open about some of the entrenched challenges specifically faced by Radiographers.
But mainly to say that…
Much of the narrative around AP is centred around the Emergency Department, Critical Care or in Primary Care. They commonly have a Nursing, Physiotherapy or Paramedic background. Many of these roles are long established and have their own framework which is used to “describe” their scope, duties and practice, and their roles seem to have little in common with Radiography at first glance.
How do you achieve AP or what is AP?
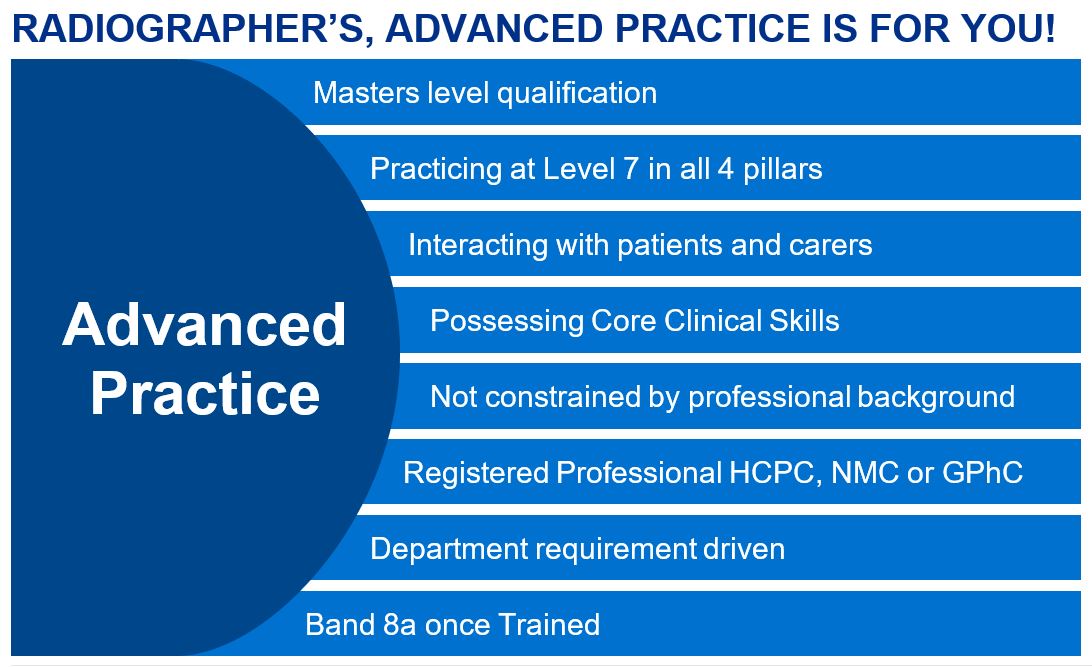
AP is a deliberately multi-professional term and job descriptions for an Advanced Practitioner should not stipulate specific professional backgrounds. The core skills required for AP are generic across all professions. The HEE definition of AP is below and covers both working at level 7 in the 4 pillars, but also interacting with the patient, relative or carer, being responsible and working autonomously for specific care episodes.
There are a number of routes into AP, apprenticeship, MSc (non-apprenticeship), and the ePortfolio (Supported) Route. The first two would apply to those who are starting their journey, and the latter to those who consider themselves Advanced Practitioners and already work at the advance practitioner requirements described in the Multi-professional framework for advanced clinical practice in England.
“Advanced clinical practice is delivered by experienced, registered health and care practitioners. It is a level of practice characterised by a high degree of autonomy and complex decision making. This is underpinned by a master’s level award or equivalent that encompasses the four pillars of clinical practice, leadership and management, education and research, with demonstration of core capabilities and area specific clinical competence. Advanced clinical practice embodies the ability to manage clinical care in partnership with individuals, families and carers. It includes the analysis and synthesis of complex problems across a range of settings, enabling innovative solutions to enhance people’s experience and improve outcomes.
Multi-professional framework for advanced clinical practice in England (pg8)
Misconceptions
One of the biggest misconceptions about AP involves non-medical prescribing (NMP). This is not a requirement of AP. It may be an advantageous skill to have, but it is not an essential requirement. Indeed, much of the work covered by NMP can be covered by Patient Group Directives or Patient specific directives, although this is more work and can be restrictive.
The other big misconception is that it doesn’t apply to my profession, i.e., radiography. Simply put, yes it does. The Multi-professional framework has been carefully constructed by key stakeholders from all professional bodies to be able to apply to ALL professional groups.
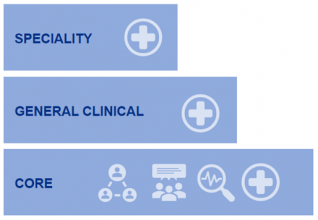
There are key requirements which are common to all and are achievable to all. (Fig3) These can be split into 3 groups, Core, Clinical and Specialty.
The core consists of teaching, research and leadership, which are common to all professions. The general clinical will encompass critical thinking, physical examination skills and understanding what the various tests mean, the final section being those clinical skills that are specific to that role.
Why Advanced Practice?
The fundamental drivers behind the provision and development of AP roles are innovation and flexibility. These allow the creation of roles with input from groups, with local expertise to address local and national healthcare requirements.

Is there funding?
YES! Organisations can apply for HEE funding for each Advanced Practice trainee for a training grant and additional educational supervision funding allocated to ensure supervision time. Scoping for funding in the South West opens each year in February for 6 weeks. The advice from HEE is to use the apprenticeship levy where possible, so tuition fees are paid for by the apprenticeship levy. This ensures that the training grant is entirely available to the employer/department. More details about the funding can be found on our website.
Sounds great, how do I apply?
The key here is to understand AP roles are there to fulfil or develop a departmental or service requirement. The department or service would apply through their Advanced Practice lead for the Trust. The Trust AP lead will ask you some questions, check you are in an Advanced Practice role, or working towards one, and all the requests for funding are sent off in the scoping window.
Why do I need to get a full MSc or Level 7 Apprenticeship to be an AP?
One of the requirements of AP is a minimum educational level, MSc in AP. This ensures a common standard curriculum across all the professional groups. The MSc in AP ensures that common core capabilities are achieved, together with the appropriate clinical skill set for the specific role. There is an accreditation framework in place which ensures that all AP’s that have completed a HEE accredited course will have an electronic badge indicating that they are a HEE recognised AP. Within the documentation on primary care assessment, the CQC is proposing to check who is accredited and who is not. This is likely to also be a requirement for secondary care in the future.
Why is this recognition important?
HEE recognition is to ensure that the level of responsibility, educational requirements, and job role, are comparable across all professional groups. This also ensure good governance is understood and enshrined in practice ensuring standardisation in quality and safety for the patient.

What do I need to do if I think I’m in an AP role?
You need to compare your job description to the Multi-professional framework, see if this matches correctly. Look at the time allocated to each aspect of the 4 pillars, HEE suggest an 80/20% split between clinical and non-clinical. It is important to note that you might be performing an AP role, as your role has grown, but your JD is not indicating that the role has changed. It would be vital to therefore get the JD amended to accurately reflect your role, otherwise you will not be in an AP role. But crucially AP roles are about identifying a service need, and filling that requirement with a suitably trained and qualified individual.
Why now?
There is a huge shortfall in the workforce that can deliver the care required, coupled with the attrition of experienced AHP staff due to dissatisfaction with the lack of current career progression. Combine this with the opening of the new diagnostic centres, this creates the environment and the requirements for radiographers to step into AP.

What are the challenges?
Acceptance: Radiographers are different in the way our roles are structured from the perceived main players such as Nurses, Paramedics and Physiotherapists. Our scope for patient contact is significantly more limited in our normal duties and with relatives and carers almost non-existent. Consequently, although our ability to match against the 4 pillars is relatively straightforward, it’s more challenging to achieve the patient interaction which completes the episode of care.
Attitude: AP gives Radiographers an opportunity to develop as professionals, however we need the vision to see how our roles fit into the AP picture, and not be constrained by the ways that we have always worked. This is exemplified by trying to create AP roles which mirror the workload of a Consultant Radiologist. Radiographers are not Radiologists and what we bring to the patient pathway will reflect that difference.
Funding: There will be established roles created under the auspices of the Agenda for Change framework as Advanced Practice Radiographer, and graded at band 7. Some of these will be correctly matched against the 4 pillars, and some will have time allocated to achieving the pillars of leadership, research and education. However, the HEE stipulate that all APs who have a role requirement to work at this level should be banded at 8a or above. To be successful in any funding application request evidence of an 8a role at the end of training is required. This creates a financial challenge to the organisation by changing the funding of a role when there may not be an obvious benefit to patient care by doing so.

Gaps in the workforce: Developing individuals into AP roles, there will be both a draw from the enhanced Practice workforce, but also from the Practitioner workforce, resulting in a lack of individuals to deliver the baseline Radiographic skills, so new or rather alder ways of achieving this must be considered. As Radiographers develop into more clinical roles accepting and earning the responsibility and clinical respect of medical colleagues, we too must look to upskilling our assistant workforce to fill the workforce gaps.
Finally
Advanced Practice is for Radiographers, and is a great opportunity to grow our profession into the next phase of its natural evolution and development. It is not with difficulties, but these are surmountable and, in some ways, advantageous. By adapting, the profession can continue to deliver the high-quality care and treatments well into the 21st century.
For more information on Advancing Practice in the South West go to our website.
Somerset Faculty of Enhanced and Advanced Practice
Julie Reeve – Consultant Nurse Emergency Medicine / Advanced Practice Project Lead Somerset STP/CCG
Somerset is a mainly rural county with a population of 0.6 million. There are thirteen Primary Care Networks and two main acute NHS provider organisations – Yeovil District Hospital (YDH) NHS Foundation Trust and Somerset Foundation Trust (SFT). SFT is a result of a merger between Taunton Foundation Trust (an acute trust) and Somerset Partnership (a community and mental health trust) in April 2020. A merger between the Somerset Foundation trust and Yeovil District Hospital NHS FT has been agreed in principle and is currently in the initial planning stage. This will result in one single NHS provider organisation serving the Somerset population.
As a result of the initial Health Education England (HEE) strategic planning and workforce modelling project, the Advanced Practice Leads and senior responsible officer (SRO) set up a Somerset Wide Faculty of Enhanced and Advanced Practice FEAP in early 2020. This expanded on the previously established FEAP at YDH. This group has representation from all key stakeholders and the chair provides the Somerset Peoples Board with updates and outcomes from the FEAP.
Somerset FEAP Membership
Director of Professional Practice and Standards (Chair)
Project Lead (Deputy Chair)
Education, Learning & Development
Primary Care
Pharmacy
Hospice
Mental Health
Symphony Healthcare Services
Yeovil District Hospital (YDH)
Somerset NHS Foundation Trust (SFT)
Nursing
Paramedics
Allied Health Professionals (AHP)
The main advantage of the FEAP is the multi professional membership which has enabled a more cohesive standardised approach to the Advanced Practice (AP) programme. Whilst some areas were more aware of AP agenda than others, the different teams and services have all continued to learn together and importantly have been able to share their positive experiences as well as their challenges, which we work through as a group.
The group members are also the champions when it comes to dissemination of information which supports the standardised approach which is so important. The group receive information from experts in the field of AP as we have guest speakers from the South West AP Faculty. We also have a project lead for AP who is a link with the other county project leads, other key groups and the FEAP. At the start of the project it was obvious that there was significant confusion around advanced and enhanced practice, and whilst we still have a way to go, having the group who are informed in the correct way, has driven the education in the same direction across the wider system.
One other key success of the FEAP was the agreement of a standardised AP band 8a job description and because the groups’ representation is so diverse, this has been shared widely. It is too early to understand the impact of that but the driver again is to promote standardisation and ensure that the roles are supported appropriately.
The Somerset FEAP has also created a multi professional directory of staff who are working in, or are in the training phase to achieve, AP status. Understanding where our AP workforce is allows more effective supervision, support and importantly networking for those in similar services. We have also started to include names of aspiring ACPs which enables us to target appropriate individuals if there is an opportunity of new AP roles within their own speciality. The aim for this work is to ensure that we can develop staff who have the desire to work in an AP role when there is not a direct opportunity in their own service. This will promote keeping senior staff within the county and ultimately will be an important part of staff recruitment and retention. This is a live document is evolving all the time and it is helping to inform the strategy for advancing practice going forward.
Establishing the FEAP has been a great driver in getting the AP role recognised and embedded in services as well as ensuring that standards are applied across Somerset. For those thinking about setting up a similar forum, it gives a voice to those working in AP, and allows for easy consistent messaging, whilst promoting the AP agenda.
NETS
A big thank you to all the AP trainees who filled in the NETS survey last November, your feedback is greatly appreciated. We received twice as many responses than we did last June. We would like this number to be an even greater one for the next survey in November!

NETS is a survey that offers students and trainees the opportunity to comment on their experience, asking them to provide feedback on what is working well and what could be improved. The results from November show that there are some supportive learning environments, but there are things that could be done better.
- 100% of AP trainees in the South West who responded had the opportunity to discuss and agree their learning needs with their supervisor.
- 92.7% of AP trainees were satisfied with their overall education
- 97.4% were satisfied with the supervision they received during their training.
- 39% of AP trainees reported workload was affecting their course.
- 97.6% of AP trainees knew how to raise concerns but 12.2% did not feel comfortable raising concerns.
- 30.8% of AP trainees were considering leaving their course. The main reasons for this were: doubting ability and feeling overwhelmed.
In response to your feedback, the SW Faculty of Advancing Practice will continue to work closely with trainees, employers, and our quality team to address the concerns raised. The Faculty will look to produce guidance on the induction process, to ensure topics such as raising concerns is covered. We will continue to engage with providers to ensure they re-evaluate themselves against the readiness to train checklist and are following plans in place to improve the learning environment within their organisation. The feeling of being overwhelmed with the workload and doubting ability (also known as imposter syndrome) is a common feeling amongst trainees, particularly those starting out. To help with this, we will continue to provide pastoral support through our Supervision and Assessment leads, as well as continue to host events that give trainees and supervisors the chance to interact and support each other across the region.
NETS will re-open in November 2022, participating is one of the ways that we can collect your feedback and make real change on areas of concern. If you are an Advancing Practice trainee / student, please fill out the survey and give us your opinion.