You will find this case study useful if you are interested in:
– Early career
– Training: HEI modules
– 4 pillars in practice
– Personal development into advanced practice
– Training: supervision
– Role impact: patient
– Advanced practice role development/creation
– Role description
– Role impact: service
Early career
My first role was within a band 5 rotational post where I completed rotations in orthopaedics, community and acute medical and surgical wards which included paediatrics and intensive care. From this post, I moved to a band 5 position within a front door team, before securing a band 6 job within that same team where I have remained for the last six years. During this time, I have developed a really keen interest in frailty and was really excited working on our older person short stay ward alongside our geriatricians. Through conversations with my manager around my enthusiasm for this area I was supported to complete the NHS England Frailty Collaborative with four or five staff members from around our hospital which focused on reducing the number of bed moves for our frailty cohort using Quality Improvement methodology.
During my early career the language of the four pillars of practice wasn’t in use and I didn’t frame my development in those terms specifically. However, I was always questioning my practice along the lines of “what can I be doing differently to make patient care better?” My personal motivation prompted me to complete audits assessing the services and care we were delivering, including the link between falls prevention and readmission and the early therapy intervention on presentation to the emergency department. I also completed the NHS Leadership Academy Edward Jenner Course and broadened my network through attendance at conferences.
Personal development into advanced practice role
I would say my advanced practice journey really started when I applied and was successful for a band 7 clinical specialist physiotherapy role for the front door team. I wanted to develop the role and help to showcase the capabilities of our team. I then became aware of a number of trainee advanced practitioners working in frailty that had recently been employed by the trust. I However, I was always questioning my practice along the lines of “what can I be doing differently to make patient care better?” I felt that if I could combine my current knowledge and experience in mobility and discharge planning, with medical assessments then I could transform patient care and their journey at the front door.
Practice role development
I could see opportunities beyond the current limits of my scope of practice and felt that, with additional training and skills, I could give a lot more in delivering care to these patients. For example, if a patient came in with a swollen arm and it was bruised, I would assess and be highly suspicious that they had a humeral fracture but there would be a bottleneck as I couldn’t request and review the x-ray, which meant a longer patient journey time. From observing other advanced practitioners, I realised that practice at this level would allow me to develop my skills and contribute to a better patient pathway and help them receive the right care, at the right time, from the right person. This would help patients to progress through the system quicker and get of out hospital sooner.
I spoke to my line manager and described my vision, where I wanted to develop, and how I saw this service evolving through the lens of advanced practice. My line manager also felt that a role like this would help showcase the service and attract new staff as well as retain current staff.
I set up a meeting with an emergency department consultant to discuss my vision for the service. They were supportive of the proposal and agreed to provide clinical supervision.
As this was a new and innovative approach within our trust, the whole process took considerable time and engagement with a range of stakeholders. I worked to be clear in my pitch, describing the rationale and benefits of developing this role. I was also aware that this development may potentially be seen as being detrimental to the base team as they would lose me and my skillset whilst I was training. I maintained my own resilience and worked with others to acknowledge the short-term difficulties but also to create a shared vision around the benefits I believed would that advance practice would realise in the long-term.
As my role was new, I used the ‘evidencing work-based learning’ module to enable me to gather the evidence and data to write a business case to generate a new post, rather than use the existing band 7 post to create the advanced practice role
I am completing my MSc in Advanced Practice through the University of West England. I chose to complete the ‘evidencing work-based learning’ module first to allow scoping and development of the role as my training and experience progresses. As this is a new and innovative role within the organisation, its development has taken considerable amounts of time and personal resilience as well as engagement with multiple stakeholders, to bring to fruition.
Training
I recognised that the full MSc was required to progress to a role as an advanced practitioner that works across all pillars. I’m currently doing the University of West England MSc in Advanced Practice. The modules I have completed are:
– Evidencing Work-Based Learning
– Leadership and Innovation
– Health and Social Care Research Methods and Methodology (pending)
– Pathophysiology and diagnostic reasoning module
– Advancing practice in clinical assessment and differential diagnosis
– Non-medical prescribing (on-going)
To select the optimum modules, I discussed the various options with other advanced practitioners working with older people. I also wanted to tailor the modules to my own clinical scope of practice as best as is possible.
Recognising that in my role I may be the first clinician to assess patients, choosing the 40 credit Advancing Practice in Clinical Assessment and Differential Diagnosis module rather than the lesser 20 credit Physical Assessment and Clinical Reasoning module to allow maximum training opportunities in these elements so better underpinning my confidence and experience was the right choice for me and my patients.
“Formulating a clear supervision structure with my clinical supervisor and regularly reviewing progress has been helpful to reflect and notice developments, not only in my clinical competence, but also my clinical confidence”
I have prioritised maintaining a focus on supervision, ensuring that I kept monthly check in meetings for reflection and taking stock. I request direct feedback about my progress. There have been challenges and bumps along the road around keeping regular supervision opportunities. Formulating a clear supervision structure with my clinical supervisor and regularly reviewing progress has been helpful to reflect and notice developments, not only in my clinical competence, but also my clinical confidence.
I started with two clinical days per week which was later reviewed; I felt that I wasn’t getting enough clinical exposure and that three days per week would work best.
Advanced practice is not a replacement for medical staff although during my training. It has been difficult at times as I’ve compared myself to the trainee doctors that I work alongside. That comparison is natural, but it is important to remember the different backgrounds of advanced practitioners compared to doctors. I’ve needed to remind myself that I have completed my physiotherapy degree and a further seven years of clinical experience, most of which has been in the assessment and management of older patients with frailty, before starting my advanced practice training.
My previous experience and knowledge have all complemented my MSc studies and is enabling me to develop the skills and confidence required of an advanced practitioner.
I have been challenged a lot and there is a huge amount of imposter syndrome that I’ve felt moving through this process, especially worrying about whether “I am working outside my scope of practice, and should I be making this decision?” Knowing I have the trust and support of my multi-disciplinary team colleagues, including the consultants, is hugely reassuring. It has been a real-life journey of self-discovery.
Role description
The role is continually evolving as my training progresses and more and more my role is becoming known and understood by the wider multi-disciplinary team.
At this point in time, on a typical shift I will attend the emergency department handover and let the emergency department consultant know that I am on shift. I have an awareness of the patients in the department and will prioritise seeing patients that are likely to also require therapy intervention. The care I give is holistic, rather than just through a therapy lens. I would ideally see patients straight from the ambulance and start the assessment of their needs as early as possible both from a medical and from a therapy perspective, but this depends on flow and medical staffing within the department. This allows earlier identification of potential issues that may otherwise delay discharge and start things in motion to have the patient admitted or transferred more quickly to a short stay ward if there is additional care that they need.
I deliver training to the emergency department nursing and medical team on frailty to enable colleagues to extend their assessment to prevent unnecessary overnight stays. I’ve also completed teaching to the therapists, covering acute coronary syndrome and renal function to help them improve their medical knowledge and their interpretation of blood biochemistry. This then helps when the therapy team are triaging their list in the morning to feel confident that a patient might not be medically fit because their bloods are deranged.
Impact and evaluation
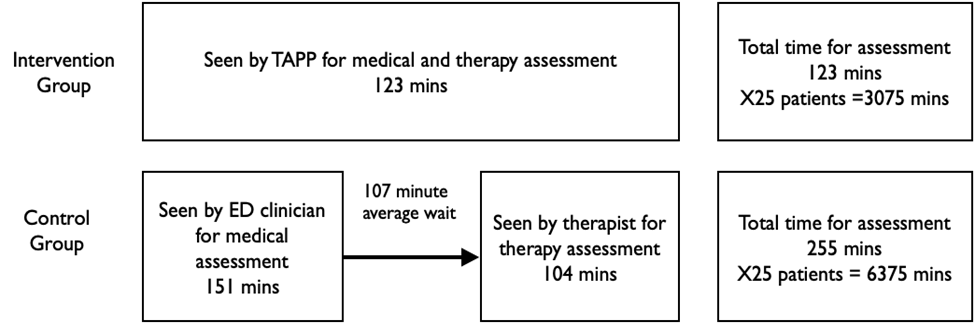
The graphic below was developed as a result of the data collection completed for my Evidencing Work-Based Learning module for my masters. It demonstrates the transformation of the patient pathway that has been made possible due to the advanced practice upskilling I have undertaken. It focuses primarily on the time taken to complete a thorough assessment incorporating both medical, therapy and social needs, with a significant reduction in assessment times from an average of 255 minutes to 123 minutes per patient. This in turn is having an impact on early frailty identification, management of patient and family expectations and early discharge planning conversations.
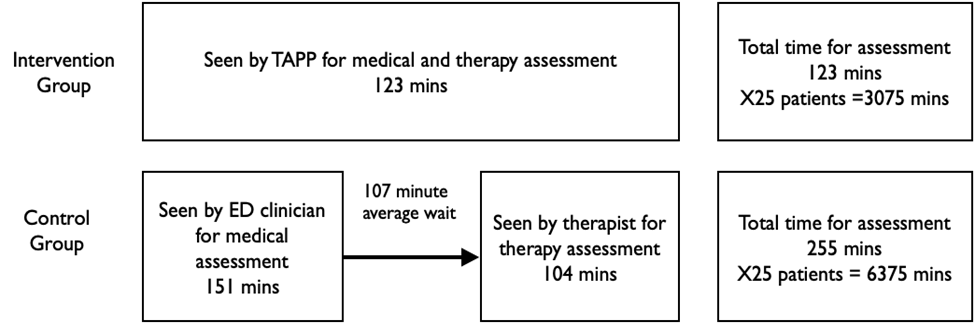
This has secondary effects in that ambulance crew can be released back into circulation and bed managers are aware of possible admissions much earlier in the process so their planning and decision-making gains clarity. This then influences bed capacity and can help improve the accuracy of other decision at the hospital operations level.
The feedback that I’ve had certainly from my medical colleagues is that they have often preferred that I see some of “their” patients as they feel I can deliver a more holistic and frailty focused assessment that a medical colleague who is primarily there from emergency department and may have limited frailty or older person experience. This feedback has been really reassuring as initially I was worried that my role would be seen as encroaching on their territory somehow, but they have been really supportive.
As the role develops, my research energies are focused on continuing to define exactly what the role should look like once I have completed my training for maximum patient and service benefit.
In the future, I believe that I can provide the leadership and education to develop a standardised process that links from the community/primary care setting through to the older persons’ wards. I also have an interest in continuing to scope where else roles at an advanced practice level could be implemented to improve patient services.