
Amy is a trainee Advanced Practitioner working in the Emergency Department with a specialist focus on soft tissue injuries. Amy is a Physiotherapist by background and currently completing her Masters of Sciences (MSc) in Advanced Practice.
Why did you want to become an Advanced Practitioner?
I had started in a role in the Emergency Department as a Physiotherapist but could see the potential for improvement for patients being admitted with soft tissue injuries who often experience long waits, both within the Emergency Department and for onward advice and care.
| Amy works at Level 7 across the four pillars of advanced practice |
|---|
| Clinical – Advanced clinical response to patients with soft tissue injuries who present at A&E – Streamlining care, preventing re-admission and improving quality and experience |
| Leadership – Creating and sharing the vision for this pioneering service – Developing clinical leadership skills |
| Education – Invited to teach a MSc module at an HEI – Offer clinical supervision, support and training to nurse practitioners, junior doctors and students |
| Research – Respond to service needs and demands relating to audit and research – Member of a regional group to help disseminate best practice – Completing MSc in Advanced Practice |
These waits for onward care can cause an individual injury to become a chronic (long-term) problem which can have an impact on a person’s ability to work and/or mental health. Training as an Advanced Practitioner is a great way to give immediate expert care and make sure our patients can get back to normal life as soon as possible.
What is the best thing about your training?
Being able to broaden the scope of my assessment; it was previously frustrating when I needed to pass patients on for further assessment which would prolong their time in the emergency department and mean they must repeat their story to another practitioner.
Why is Advanced Practice good for patients?
Data from the pilot of this role in ED showed patients experienced a lower than average waiting time, reduced reattendance rates and increased patient satisfaction (100% on friends and family test) when seen in ED by an Advanced Physiotherapy Practitioner
Feedback from a patient “Instant results and amazing examination and explanation of injury, treatment and effects. Amazing member of staff “
I can provide immediate expert assessment to patients attending the Emergency Department with soft tissue injuries, giving accurate diagnosis and a treatment plan that works towards long-term recovery, rather than only addressing the immediate symptoms. The skills I have learned during my Advanced Practice MSc allow me to address any additional needs they have within one consultation, e.g. head injuries or closing wounds which reduces the need to see multiple members of the team.
How do you see your future as an Advanced Practitioner?
I would like to use my skills in leadership, education and research to look across patient pathways such as fractures, sports injuries and orthopaedics; to keep looking for new ways of working and improving patient care.
Feedback from a colleague “We have found great value and benefit from the advanced physio practitioner service. From a clinical perspective and also from a teaching and access to peer advice perspective. The Advanced Physio Practitioners offer expert knowledge on consultation on a wide variety of presentations and are constantly expanding scope. This delivers an expert level of care for MSK presentations and reduces re-attendance rates.”
Want to read more about Amy? Click here to open a more detailed interview.
You will find this useful if you are interested in:
– Early career
– Role description
– Personal development into advanced practice
– 4 pillars in practice
– Advanced practice role development/creation
– Training: HEI modules
– Role impact: Service
Early career
My undergraduate degree was in sport and exercise science in Birmingham. I’m a triathlete and the relationship between health and fitness has always interested me. I originally wanted to go into medicine but realised that Physiotherapy allowed me to encompass my interests and think about how I could improve quality of life and participation in sport and being active. I went on to do the pre-registration Masters in Physiotherapy at Kings College in London.
My first role was on the Band 5 rotation in Royal United Hospitals Bath, covering Elderly Care, Surgery and Medicine, on-call Respiratory, Musculoskeletal and Intensive Care. From here, I moved into a Band 6 rotation, again covering Elderly Care, Rheumatology and Musculoskeletal outpatients. Throughout, I had discussions with colleagues about my skills and progression, understanding my gaps and opportunities. I didn’t cover Neurology within my Band 5 rotation, and so sought opportunities in my Band 6 role to experience neurological conditions and assessments, for example, alongside the spinal team. Working in this reflective way has enabled me to accelerate my career and seek out new experiences despite my feelings of imposter syndrome!
When the COVID-19 pandemic hit, I was redeployed to work in Intensive Care, using my experience from the on-call respiratory rota. I volunteered for this due to the brilliant physiotherapy team lead who inspired me as a leader and who I wanted to work alongside. I was given responsibilities which grew my skills and confidence in leadership and made me feel ready to progress. I enjoyed working holistically across the medical and psychosocial sides of care and working as part of the wider and multi-professional team. I also saw that the NHS can develop new ways of working at a pace and that I had skills for thinking outside the box and setting up services.
Personal Development into Advanced Practice
It was identified that there was a need to improve soft tissue injury management in the Emergency Department. A physiotherapy colleague, Head of Therapies and Matron created a business case, and a role was created to set up a physiotherapy service in the Emergency Department. For me, this seemed the perfect way to combine multi-professional team working with my love of Musculoskeletal conditions. I applied and was successful for one of the two newly created roles. At the initiation of the service, the role was advertised as Physiotherapy Practitioner, working alongside the nurse practitioners, rather than an Advanced Practice trainee.
Within the role, I started my prescribing module. Through further conversations with our head of therapies, we discussed that the service leadership, clinical skills and innovative nature of this role were aligning with advanced practice, and NHS England Workforce, Training and Education funding was sought for the Advanced Practice training.
Training
I’m partway through my Advanced Practice training, with 4 out of 7 modules completed.
Modules completed so far:
– Prescribing
– Pathophysiology and Diagnostic Reasoning
– Physical Assessment and Clinical Reasoning
– Leadership
Upcoming:
– Research Methods
– Evidencing Work Based learning
– Dissertation
The first year in urgent care with this training has been great to consolidate learning. Lots of the modules are broad, covering head injury, abdominal pain, cardiovascular, ENT etc. which I’ve really enjoyed; I can see how it will benefit my assessment. I have previously found it frustrating when I was able to assess some of the patient’s needs and then pass them on. Now, I’m reaching the point where I can manage the soft tissue injury, but also assess the head injury, suture the wound and see the episode of care from start to finish and getting so much job satisfaction from this. In the prescribing module, I’ve learned about drugs that I’m unlikely to ever use, but the awareness is important when a patient tells you the medications they are on and you need to know what the side effects and interactions might be.
Development of Advanced Practice role
Going on the Advanced Practice course has started to then influence the shape of my role. This is still forming and leading to interesting conversations within our services. Having these additional skills allows me to work beyond my original scope and take more autonomy over the patient pathway. It has also created discussions around the difference between my role and the nurse practitioners and the blurring of lines; should we become more general practitioners or act as a separate service working alongside them?
For me, I think there is value in having specific areas of expertise for patient outcomes. The role came from patients who were experiencing poor outcomes and this needed addressing; through our pilot, we gathered evidence through patient satisfaction scores and outcomes which showed that they valued that broader level of expert assessment, diagnosis and management within the Emergency Department. Previously, these patients would have received a referral and then could have waited up to 6 weeks or more for a specialist assessment.
I have liaised with the Chartered Society of Physiotherapy about prescribing rights. We are currently using a mix of independent prescribing and Patient Group Directives which is working well but is also creating a blurring of boundaries. Part of the development of the role will be working through these and educating others.
The governance of this role is key; at present we are maintaining a tight scope of practice and insight into how we’re developing our competencies. It can feel tempting to stretch that when the department is under pressure, but I’ve got better at saying no, only seeing those I can see safely with my current skills.
Role description
Previous patient pathway:
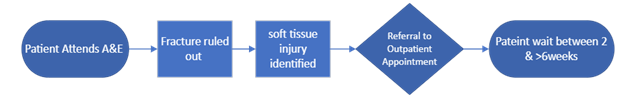
Outcome:
• May be diagnosed but given limited, non-specialist advice and management for their condition.
• May not be accurately diagnosed, leading to long waits for diagnosis and consequent treatment.
Longer waits for accurate diagnosis and treatment result in:
• Delays to rehab
• Worsening of injury
• Reduced range of movement and power (deconditioning)
• Delayed access to surgery
• Mental health impact
• Financial loss to patient, access to work. Reattendance to ED, Increased risk of condition chronicity
For NHS services, this can result in a higher burden on services later on, e.g. through avoidable surgeries and repeat presentations at the Emergency Department. Repeat presentations can often occur because of patients’ poor understanding of recovery times for soft tissue injuries; when expectations aren’t managed at the outset, patients will access services again with concern that things aren’t improving rapidly.
Patient pathway with Soft Tissue Trainee Advanced Practitioner
All patients are seen by the triage nurse as they come in. Each practitioner looks at the list and picks the next patient that comes within their skill set. I select patients whose primary need appears to be soft tissue related, although I will concurrently manage any other injuries or illnesses that they present with, for example, head injury, ordering and interpreting blood tests, prescribing, suturing etc.

Proudest clinical moment
A patient was escalated to me due to pain in both legs (sciatica). Through specific questioning, I was able to identify red flags that she had not passed urine for some time and was in urinary retention. I discussed with the Consultant, explained my findings and requested an MRI. MRI reports confirmed spinal cord compression called cauda equina. In this instance, specific questioning and differentiation from the suspected sciatica across both legs, given as the provisional diagnosis, was key.
Without this assessment at this stage, she would likely have been sent home with spinal cord compression, potentially with a very poor prognosis. As a result, she may have been at risk of becoming a ‘revolving door’ patient; continuing to present to healthcare professionals whilst being at risk of severe deterioration.
4 pillars in practice
Alongside the clinical skills above, the pilot has encompassed the other 3 pillars of advanced practice; it is difficult to separate them out as they all work so intrinsically together in practice.
• Research
For research, we are linking with services in other areas to define what good looks like. I’m a member of a South West regional group of Physiotherapy Practitioners in Emergency Departments that shares support around research. I’ve used this support to help audit and develop the service that we needed. Running the pilot alongside undertaking my studies in Advanced Practice worked hand in hand to benefit both elements.
• Education
I offer clinical supervision and support to nurse practitioners, junior doctors and students from all professions. I am also offering training to the nursing and medical teams on soft tissue injuries. Within the education pillar, I’m always looking at best practices and the most current evidence for assessment and management, which in turn keeps me up to date.
I’ve also been approached by UWE to do teaching on the ‘APiCa’ course for nurse practitioners which I’m exploring for next year.
• Leadership
Within this role, I am setting the vision and leadership for this pioneering service in this setting. I am applying my leadership skills every day to continue to develop a service which will be the best it can be for our patients.
Role impact
We are demonstrating the benefit of having an expert, holistic skill set for this patient group. There’s understandably a huge amount of pressure around the life-threatening injuries in Emergency Department majors, which obviously need to take priority. This can lead to more minor cases, including soft tissue injuries experiencing long waits, receiving an initial assessment and then being referred for onward assessment and care. Within my previous outpatient role, I saw the impact of this, when patients hadn’t had treatment for over 3 months, by which point their condition was chronic. Chronic problems can have a significant psychosocial impact; mental health can deteriorate, access to work is affected, people can withdraw socially and stop functioning and participating as they did prior to their injury.
In my role, I ensure that patients get the right diagnosis at the right time and the right management on day one so that they can feel confident about self-managing their injury. This allows them to get back to work, engage in what they want to be doing and resume a normal quality of life.
I have worked with the business intelligence team to gather data on the service, based on Emergency Department’s Key Performance Indicators. Patients who accessed our service had
• An average waiting time of 47 minutes (the national median is 55 minutes)
• Lower than average total time spent in ED (126 mins versus 136 mins)
• A reattendance rate of 2% (national rate of 9%)
• Fewer than 3.5% breach the 4-hour target
• 100% patient feedback of ‘very good’ on the family and friends test
We are also receiving ‘on the ground’ feedback from physiotherapy teams that less physio rehabilitation is required further down the pathway and surgeries have been avoided through timely rehab.
Patient quotes:
“Instant results and amazing examination and explanation of injury, treatment and effects. Amazing member of staff”
“Great experience […] for a potential stress fracture today. Advice on exercise load, fuelling and management that allows me to stay active.”
Vision for the future
There are currently 2 advanced practitioners offering a 7-day service.
Although the service is currently run by two physiotherapists, these roles in the future could be developed into multi-professional opportunities for others with knowledge and skills in this area. Succession planning is key to ensure service sustainability, including support for staff at a band 6 level and trainee advanced practice positions.
My vision would be to expand the service to have a greater number of staff who could follow patient pathways such as fracture, sports injuries and orthopaedics. Particular pathways such as back pain could benefit greatly from work at an Advanced Practice level.
I would also like to explore outpatient departments being able to bleep us in ED, for example, if DVT is suspected for immediate assessment and treatment.
There is great future potential for research projects. The outpatient team are doing some research on prehab for ACL (knee ligament) patients and we’re linking with them on this.
Read more advanced practice case studies from the South West region here