Understanding the impact of healthcare roles is crucial for improving patient outcomes, optimising resource allocation and ensuring accountability within healthcare systems. It allows for evidence-based decision-making, demonstrates the effectiveness of interventions & roles, and provides insights for continuous improvement.
There is a particular focus for us on considering the impact of advanced practice, especially as roles emerge in new and novel areas of practice. This helps us to understand the benefits that these roles bring to patients, pathways, services and systems.
What do we mean by impact:
Impact is defined as the effect or change over time that we can see, demonstrate, measure or capture on different stakeholders, and which happens as a result of an activity or an organisation. (Campillo et al 2023)
When we think of impacts, we often categorise them in to two groups:
- Qualitative: Rich, descriptive insights from open-ended feedback, useful for understanding experiences and emotions.
- Quantitative: Numerical data, often gathered via standardised tools and questionnaires, useful for tracking trends and comparisons.
We recognise that there is a difference between an ‘output’ and an ‘impact’, although they are closely related. An output is the result of a programme, intervention or activity. For example, an output might be an increased number of appointments within a service due to redesign led by an Advanced Practitioner. The impact is that patients have a reduced waiting time for an appointment.
Who do we impact on?
When considering impact, we need to consider who our stakeholders are? Who are the people we are trying to impact on? Our first thought is often to our patients and service users, along with their families and carers. However, we may also have an impact for colleagues, both in our own teams and in partner organisations.
In considering your stakeholders, you might look at where your team or service sits within the wider health system. Who do you have relationships with? Who do you spend time with or communicate with as part of your role?
A process:
It is helpful to protect some time to think about your approach to exploring impact, and the following process may help you in your reflections:
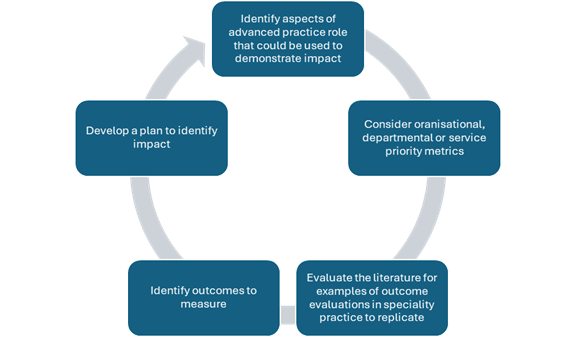
Adapted from Kleinpell (2022), pp. xvii
Outcome metrics or measures:
The outcome measures you use may be specific to your area of practice. You may like to consider the data you already gather and how this may be used to show impact.
Some areas to consider include:
- Satisfaction surveys and patient feedback
- Clinical outcomes
- Efficiency (time saving)
- Financial outcomes so as cost of care
- Benchmarking – indicating improvement when compared to national indicators
- Symptom control
- Length of stay
- Rates of adverse events
- Patient/family knowledge
- Staff knowledge
- Readmission rate
- Physical intervention use
- Adherence to best practice
- Infection rates
- Training feedback
- 360 feedback from colleagues
Tools you could use:
While we are signposting to these resources, this should not be considered an endorsement by NHS England. They are tools which might help you when exploring impact –
- If you’re doing something novel which isn’t linked with clear indicators or measures, you could explore the Most Significant Change (MSC) approach (Davies and Dart 2005). MSC is a form of participatory monitoring and evaluation which involves the collection and selection of stories of change, produced by programme or project stakeholders:
References
Campillo, I., Nunes, G. and Puertas, I., 2023. Defining impact: a shift in thinking, acting and being. Available at: www.timeshighereducation.com/campus/defining-impact-shift-thinking-acting-and-being
Davies, R. and Dart, J., 2005. The ‘Most Significant Change’ (MSC) Technique: A guide to its use. Available at: www.mande.co.uk/wp-content/uploads/2018/01/MSCGuide.pdf
Gerrish, K., McDonnell, A. and Kennedy, F., 2011. Capturing impact: A practical toolkit for nurse consultants. Available at: https://research.shu.ac.uk/hwb/ncimpact/
Kleinpell, R.M. (Ed.), 2022. Outcome assessment in Advanced Practice Nursing (5th Edition). New York: Springer Publishing
Snaith, B., Williams, S., Taylor, K., Tsang, Y., Kelly, J. and Woznitza, N., 2018. ‘Is a nurse consultant impact toolkit relevant and transferrable to the radiography profession? An evaluation project’. Radiography, 24(3), pp. 257-261. doi: 10.1016/j.radi.2018.05.001.