Updated: November 2025
Forward
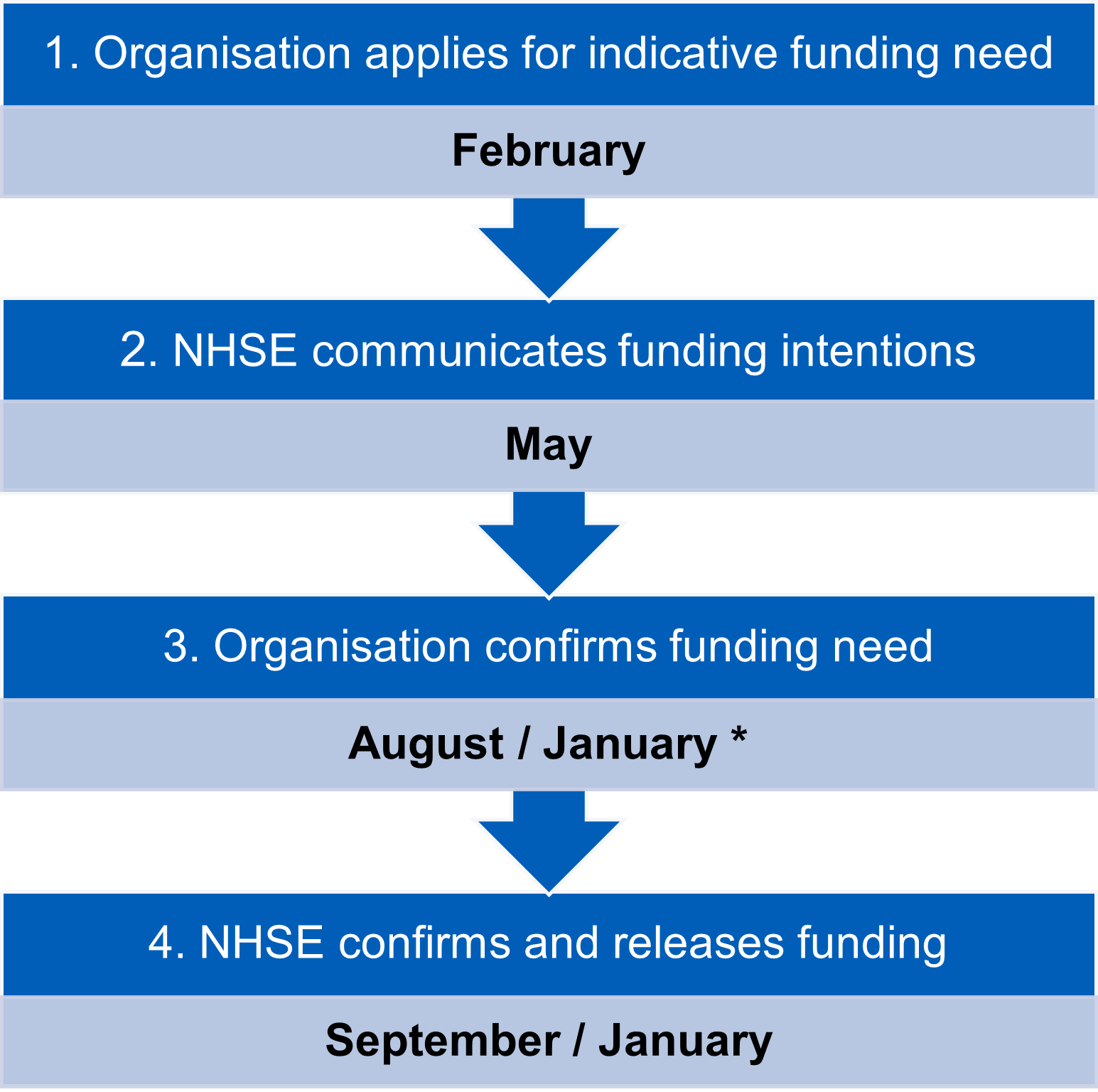
This advancing practice guidance document is designed to support regional organisations in developing advanced practice services and growing the advanced practice workforce of the future across the East of England.
The NHS Long Term Workforce Plan (2023) clearly articulates the continued drive to develop the advancing practice workforce as part of the multi-disciplinary team, recognising the impact these roles can have not only on improving patient care, but also increasing the number of senior clinical decision makers within the NHS to improve productivity and increase capacity. The plan acknowledges the role advanced practitioners will have in supporting and driving service transformation with new and innovative ways of working. It also recognises the importance of retaining our experienced senior staff and enabling effective career development where staff feel valued, entrusted and have the knowledge, skills and ability to provide high quality, safe, effective care for our patients and their families. The NHS 10 Year Plan (2025) acknowledges the importance of developing advanced practice roles as a strategy to support a new model of care that is fit for the future.
The NHS England – East of England Faculty for Advancing Practice’s (hereby referred to as Faculty) investment is aligned to the NHS England Workforce, Training and Education Delivery Plan, NHS People Plan (2020), NHS Long Term Workforce Plan (2023), and the NHS 10 Year Plan (2025). This is to ensure that across the East of England our development is responsive to system needs and will deliver the right number of staff, with the right skills, values and behaviours, at the right time and in the right place. To grow our advanced practice workforce, we will continue to work with our key stakeholders, including our Integrated Care Boards, partner organisations and education providers to identify advanced practice workforce demand, support the transformation of patient care and to invest in advanced practice workforce education and training development.
As a Faculty we are passionate about developing a multi-professional advanced practice workforce that meets the needs of the people we serve across our region. We will continue to showcase the significant impact trainee, advanced and consultant practitioners have on delivering high quality patient care and ensure we develop a culture where our advanced practitioners’ experience, expertise, and professionalism is recognised and valued. As a region we have made significant progress over the past four years in gaining recognition for our advanced practice workforce, which has only been achieved with the support and collaborative working with all our partner organisations and we look forward to continuing to work with our systems to drive the advancing practice agenda forward over the coming years.
East of England Faculty for Advancing Practice
You can find out more about the Faculty team, our priorities, additional resources and news and events via our webpage:
Visit our East of England Faculty homepage
Sign up to our East of England Faculty mailing list
If you have any questions about any of the information provided, or if you require support with the development of your advancing practice workforce, please contact the Faculty via our email: england.eoeapfaculty@nhs.net.
Contents

Download a full PDF version of this information

Q 1.1 What is advance practice?
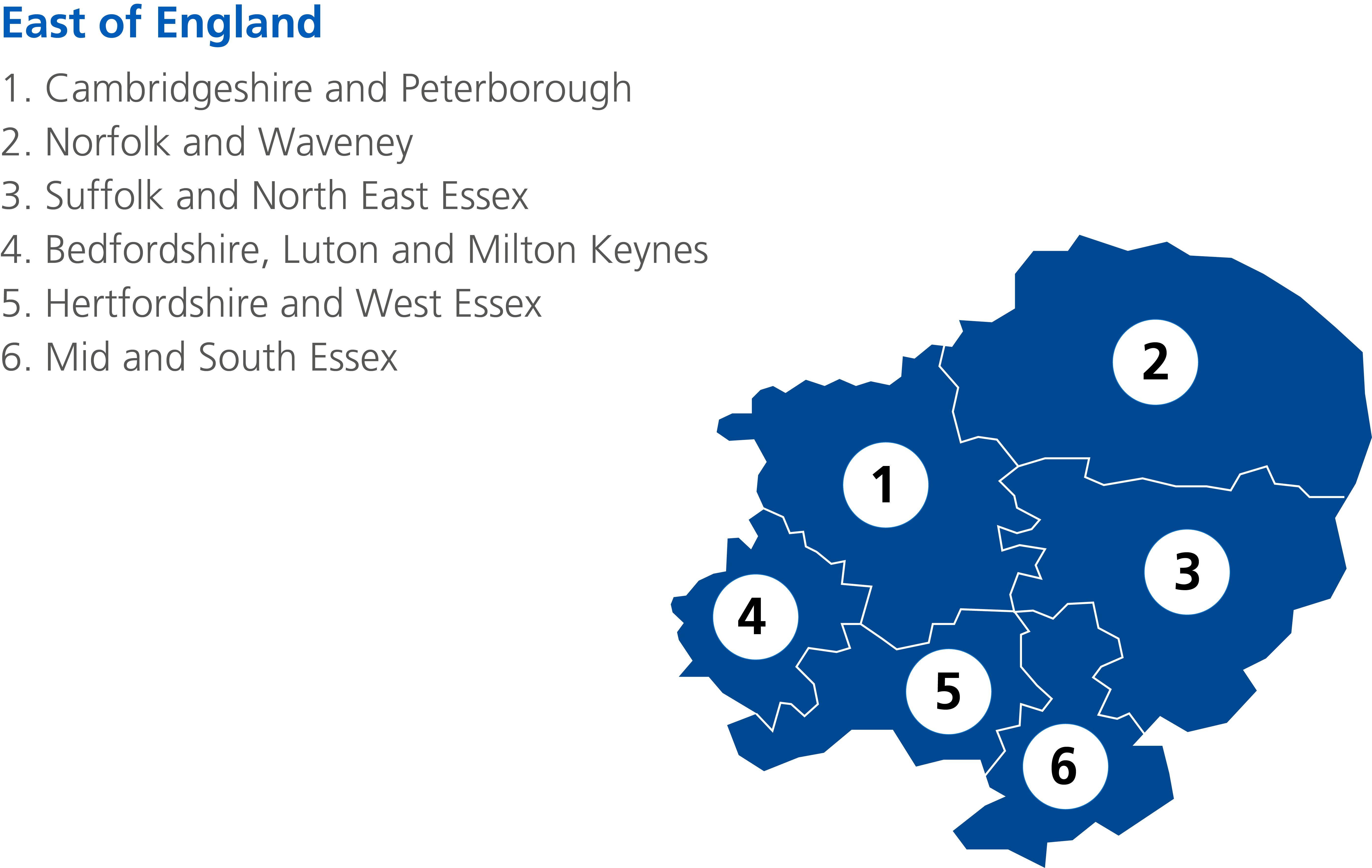
Answer: Advanced practice is delivered by experienced, registered health care practitioners. It is a level of practice characterised by a high degree of autonomy and complex decision making. This is underpinned by a post graduate master’s level award or equivalent that encompasses the four pillars of clinical practice, leadership and management, education, and research, with demonstration of area specific clinical competence. The Multi-professional framework for advanced practice in England provides a clear definition and consistent approach to the development of advanced practice across England. All health and care professionals working at advanced practice level should ensure that their knowledge and skills meet the standards outlined within the framework.
“Advanced practice is delivered by accomplished registered health and care professionals. It is a level of practice characterised by a high degree of autonomy and designated responsibility for complex decision making. This is underpinned by a post-registration master’s level award or equivalent undertaken by an experienced practitioner that encompasses all four pillars of clinical practice, leadership and management, education, and research. Advanced practice embodies the ability to manage care in partnership with individuals, families, and carers. It includes the analysis and synthesis of complex problems, and management of clinical risk and uncertainty across a range of settings, enabling innovative solutions to expedite access to care, optimise people’s experiences, and improve outcomes.”
Diagram 1– The four pillars of advanced practice
Q 1.2 Is an advanced practitioner a specialist practitioner?
Answer: No, advanced practice is different from specialist practice. Specialists are experts in their chosen clinical area, for example in diabetes or asthma care and have a depth of competencies in that specific area. Advanced practitioners have a breadth of competencies and capabilities that extend across the four pillars of advanced practice (clinical practice, leadership & management, education, research – see Diagram 1). It should however be noted that advanced practitioners may work in either generalist or specialist areas of practice, and the two roles are therefore not mutually exclusive. Services may need both specialist and advanced practitioners to provide optimum care to patients.
The table in Appendix 1 gives a high-level overview of enhanced and advanced levels of practice.
Q 1.3 What is a trainee advanced practitioner?
Answer: A trainee advanced practitioner is an experienced healthcare professional employed in a funded training post specifically to undertake the required training to work at advanced practice level. The recommended training is comprised of a NHS England Centre for Advancing Practice accredited MSc Advanced Practice programme (Level 7 study) and work-based learning to develop capabilities across the four pillars of the Multi-professional framework for advanced practice in England.

Please note: For further questions about advanced practice training, please see the Readiness for advanced practice document which can be found here.
Q 2.1 What commitment is expected of the trainee advanced practitioner whilst studying?
Answer: Trainees are required to attend education provider teaching days, practise clinical skills in the workplace and complete work-place based assessments of capabilities. Trainees must have protected time allotted to meet with supervisors regularly to plan individual educational needs and monitor progress. The requirements of supervisors are explained in more detail in the Workplace Supervision for Advanced Clinical Practice document. It is expected that each trainee will dedicate a proportion of time to independent study to become successful in achieving the qualification. The notional number of hours of study and teaching expected is approximately 100 hours per 10 academic credits (which includes both taught hours, work based learning, and independent study hours). However, the actual time spent may be more, or less, dependent on individual learners. It is therefore important for advanced practice trainees to have sufficient work-based learning time to develop advanced skills.
Q 2.2 What commitment does the trainee require from the employer?
Answer: For trainees on an MSc Advanced Practice programme, employers are expected to support the trainee(s) to meet the requirements of the programme as per the education provider requirements. The employer must provide the trainee with sufficient study leave and protected time for work-based learning per week. The advanced practice programme lead for the education provider will be able to provide information on the total amount of study days required. The employer must ensure that the trainee advanced practitioner has an appropriate co-ordinating education supervisor and associate workplace supervisors. For further information about coordinating education and associate supervisors, please refer to the Workplace Supervision for Advanced Practice (2025) guidance.
Q 2.3 What learning can a trainee advanced practitioner expect to receive?
Answer: The timetables and study time will vary according to the training route and the specific education provider, however all trainees require periods of study leave to attend educational programme and will be required to produce course work, undertake work-based assessments and produce a portfolio of evidence. Trainees may also benefit from rotations or placements in other areas within the organisation to gain the required breadth of experience.
Q 2.4 How much time will the trainee advanced practitioner be away from the job studying?
Answer: For trainees on the apprenticeship programme, the apprentice will have a minimum of 6 hours per week, irrespective of the number of hours worked per week off the job training. Apprentices must be employed for a minimum of 30 hours per week. The Gov.UK apprenticeship funding rules can be found in more detail here. For trainees on direct-entry MSc Advanced Practice programmes, employers are expected to provide the trainee with sufficient study leave and protected time for work-based learning per week. The advanced practice programme lead will provide information on the total amount of study days required.
Q 2.5 What are the minimum hours a trainee advanced practitioner must be employed?
Answer: For trainees on the apprenticeship programme a minimum of 30 hours per week is required. For direct-entry MSc Advanced Practice programmes, this will vary for each education provider, however, the general recommended amount is in line with the apprenticeship requirement of 30 hours. If the employer is recruiting a new trainee advanced practitioner, then it is suggested it is for a minimum contract of 30 hours. For existing employees who work less than 30 hours per week, it is advised that the organisational advanced practice lead and relevant advanced practice programme lead at the education provider is contacted to discuss suitability for the programme.
Q 2.6 I understand advanced practice training can include a prescribing element, what happens if I already have it, or I don’t need it?
Answer: If a practitioner already has the prescribing qualification, or it is not scope of practice requirement, then the education provider is likely to provide a choice of module(s) that the trainee can undertake instead with employer agreement. An independent prescribing qualification is not an essential requirement for an advanced practitioner, but the advanced practitioner job description may dictate that prescribing is necessary in a particular role.
Q 2.7 I have been asked to supervise a trainee advanced practitioner, how do I know if I am the right person?
Answer: Supervision is an essential element of advanced practice training. To supervise a trainee advanced practitioner it is important to have adequate experience, knowledge and expertise to provide good quality supervision. The Advanced Practice Supervisor Capabilities set out the learning and development principles for practitioners who are supervising colleagues progressing towards advanced level practice. These resources should be considered in conjunction with the Centre for Advancing Practice supervision guidance and minimum standard documents.
Q 2.8 What supervision is required?
Answer: Good workplace-based supervision is key for successful completion of advanced practice training. Trainees not receiving adequate supervision may struggle with certain modules or even completing the programme. Each trainee advanced practitioner requires a named workplace co-ordinating educational supervisor and should have access to associate supervisors who will undertake multi-professional supervision and is familiar with the learning requirements of advanced practice. Supervisors must have protected time in their job plan to support the trainee. Trainees must have time to meet with supervisors regularly to plan individual educational needs and monitor progress. National guidelines on advanced practice supervision can be accessed here.


Q 3.1 How do I know if I need an advanced practitioner role within my service?
Answer: The development of an advanced practitioner role should initially be driven by an analysis of service need and scrutiny of the capabilities and capacity of the existing and available workforce. The development of advanced practice roles should be inextricably linked to workforce development plans, which identify where advanced practice will have the greatest benefit and impact in a person’s journey through health and care pathways. This will also highlight advanced practice roles that already exist or require development in a way which meets population needs, and service demand.
Within your organisation there may be staff already working:
- at advanced level but using different job titles
- with advanced level job titles but are not meeting the principles and capabilities set out in the Multi-professional framework for advanced practice in England.
We advise working with operations/clinical managers and workforce information teams to identify what, if any, advanced practice workforce currently exists, and how they are deployed. For governance reasons, it is important to review whether existing advanced practice staff are working to the minimum capabilities set out in the Multi-professional framework for advanced practice in England.
Q 3.2 How do I develop an advanced practitioner role?
Answer: The advanced practice lead in your organisation should be aware of staff currently working in advanced practice roles and should be able to help managers understand the need for these roles and how they will transform services. To establish advanced practice roles, a clearly articulated business case for this investment is required, in collaboration with your advanced practice lead, to consider population and system needs. Job descriptions should be mapped to the Multi-professional framework for advanced practice in England and job plans should support the four pillars of advanced practice. A generic advanced practice job description and person specification is available here.
The South West Faculty for Advancing Practice have produced the Advancing Practice in Emerging Areas Workforce Transformation Resource. This resource is designed to be implemented locally by Integrated Care Systems or organisations and aims to support and standardise the approach to workforce transformation for advanced practice in emerging areas.
Q 3.3 What are the benefits and potential impact of advanced practitioners?
Answer: The NHS Long Term Workforce Plan (2023) clearly articulates the continued drive to develop the advancing practice workforce as part of the multi-disciplinary team, recognising the impact these roles can have not only on improving patient care, but also increasing the number of senior clinical decision makers within the NHS to improve productivity and increase capacity. It acknowledges the role advanced practitioners will have in supporting and driving service transformation and developing new and innovative ways of working. As well as the importance of retaining our experienced senior staff and enabling effective career development where staff feel valued, entrusted and have the knowledge, skills and ability to provide high quality, safe, effective care for our patients and their families.
NHS England acknowledges that by embracing the continued development of advanced practitioners across our organisations it will enable us to further improve the standards of care that we provide our patients by:
- Retaining valued, experienced staff who wish to remain clinically facing and still be able to advance their career thereby maximising clinical career progression opportunities. Realise the full scope of practice within and across each profession.
- Increase the focus on person-centred care, self-care, population health approaches and rehabilitation, keeping people at home, in work or school and as independent as possible.
- Improve continuity of care, discharge processes, and access to services.
- Increase capacity to supervise and develop the multi-professional workforce, to maximise scope of practice, service productivity and innovation.
- Support service redesign and transformation.
- Support teams to develop increased decision-making capability and capacity, including that required to delivery 24/7 services, improve patient/service user and carer satisfaction and associated outcomes.
- Reducing spend on temporary staff with increased safety, productivity, and value of investing in an organisations own staff.
Q 3.4 What key indicators should be included in a robust business case?
Answer: It is advised that the following questions are answered as part of the development of a robust business case:
- What outcomes are expected from the advanced practice role?
- When will these outcomes be achieved and how will these be measured pre and post implementation?
- What risks and unintended consequences might there be to the introduction of this role and how may they be mitigated against?
- What resources and support are required for role development and succession planning? (clearly include any work based supervision requirements)
- Is workforce optimised to ensure clinical and financial benefits are maximised?
- How will on-going competence and capability be reviewed and enabled?
- What reporting and line management structure will be in place?
- Has a quality assurance model been considered to measure this e.g., CQC 5 key lines of enquiry which will support inspection?
It is advised that employing organisations who currently have, or are considering advanced practice roles undertake The NHS England Centre for Advancing Practice Governance Maturity Matrix. The matrix encourages discussion and constructive challenge, as well as internal and system-wide collaboration to support the consistent implementation of advanced practice in the NHS. Using the matrix is not mandatory, but we encourage employers to utilise the self-assessment tool and connect with colleagues who have made progress with assessing and improving outcomes for advanced practice. The matrix is designed for use across all NHS settings including acute, community, mental health and primary care to strengthen governance arrangements and optimise how advanced practice roles contribute to workforce development, service delivery, and improved patient care.
Recruitment
Advanced practice embodies the ability to manage clinical care in partnership with individuals, families, and carers. It includes the analysis and synthesis of complex problems across a range of settings, enabling innovative solutions to enrich people’s experience and improve outcome. Therefore, the recruitment process for trainee/advanced practitioner posts should be robust and assess the suitability of the applicant in terms of professional knowledge and experience, academic eligibility, and personal attributes and values.
Q 3.5 What are the essential requirements when applying for a trainee advanced practitioner post?
Answer:
- Hold a current statutory professional healthcare registration.
- Extensive experience post registration and in the relevant specialty area. A minimum of 3 years clinical experience post registration with a further 2 years within the specialty area is recommended.
- Ability to study at master’s level and associated academic qualifications for role within a set time frame; this includes both clinical and academic criteria for advanced practitioner.
- Clinicians with limited degree level study will require discussion with the education provider to assess suitability to study at master’s level. Apprenticeship requirements also state the need for level 2 (GCSE or equivalent) maths and English.
Q 3.6 What is the recommended recruitment process to ensure fair and equitable appointment into trainee/advanced practitioners posts?
Answer:
- Shortlisting and interview panel should as a minimum include a senior clinician, organisational advanced practice lead or equivalent and managerial representation. It may also be helpful to include education provider advanced practice programme leads within the recruitment process
- Review NHSE – East of England No More Tick Boxes (2021) section 3 ‘Putting a different approach into practice’ to ensure fair recruitment processes are followed
- Following selection, candidates may ask for feedback relating to their profile and/or performance at the interview which will be provided by those involved in the interview process
- Successful applicants considered to have relevant prior experience will have their evidence mapped to the relevant curricula/capabilities identifying any gaps where additional training is required along with appropriate banding level, (if applicable)

Funding options and requirements
Please note: For further questions about funding options and requirements which are not answered here, please see the NHS England East of England advanced practice training funding FAQ document which can be found here.
Q 4.1 What funding is available for advanced practice training?
Answer: As of 1 April 2024, all NHSE – East of England funding for advanced practice training for new trainees is in the form of a training grant paid directly to the employer. The funding options detailed in the table below are available for new advanced practice training funding applications (continuing trainees will remain on previously agreed funding models). Regardless of funding option, £2,600 of the total training grant paid each year must be used to support clinical supervision.
Table 1 – NHSE – East of England advanced practice funding options
|
Funding name |
Funding type |
Annual £ amount |
Length of funding |
Total £ amount |
|
Advanced practice MSc – 1 year (60 credits or less) |
Training grant |
£10,200
|
12 months |
£10,200 |
|
Advanced practice MSc – 2 years (more than 60 but less than 120 credits) |
Training grant |
£10,200
|
24 months |
£20,400 |
|
Advanced practice MSc – 3 years (120 credits up to 180) |
Training grant |
£10,200
|
36 months |
£30,600 |
Q 4.2 What funding is available for surgical care practitioner training?
Answer: Currently, the Faculty are responsible for funding surgical care practitioner training. This is subject to change in future finance years; the funding options and the team responsible for this within NHSE – East of England may alter. The current funding option for new surgical care practitioner trainees is detailed in table below (continuing trainees will remain on previously agreed funding models).
Table 2 – NHSE – East of England surgical care practitioner funding options
|
Funding name |
Funding type |
Annual £ amount |
Length of funding |
Total £ amount |
|
Surgical care practitioner MSc |
Training grant |
£6,120 |
24 months |
£12,240 |
Q 4.3 What programmes are funded?
Answer: Only advanced practice programmes that will result in an MSc (level 7) award and have either been accredited by the NHSE Centre for Advancing Practice or map to the Multi-professional framework for advanced practice in England will be funded by the Faculty.
The Faculty will consider funding programmes outside of region if in England, however a valid reason for not choosing a local education provider must be provided when applying for funding.
Q 4.4 What are the requirements to receive funding?
Answer: There are certain requirements that an employer, the advanced practice trainee and the preferred training programme must meet before a successful funding application can be submitted to the Faculty. Please refer to table 3.
Table 3 – Funding requirements
|
Employer |
Programme |
Trainee |
|
Provides an advanced practice training post during training Guarantees an advanced practice post on trainee qualification Provides clinical support and supervision Provides a named co-ordinating educational supervisor and supervision plan Provides a positive learning environment Has an identified advanced practice lead |
Is accredited by the Centre for Advancing Practice, or Is an advanced practice MSc that maps to the Multi-professional framework for advanced practice If out of region, has a valid reason why a local programme has not been chosen i.e. it is a speciality programme not provided in region
|
Meets entry criteria of chosen advanced practice programme Has a substantive contract with an employer who directly provides NHS commissioned services Works in an NHS commissioned service Will complete the NHS England trainee monitoring survey Will complete the National Education & Training Survey (NETS) Not undertaking the NHS England ePortfolio route*
|
*The NHS England ePortfolio route is a funded route for experienced advanced practitioners seeking to acquire NHS England recognition that their existing education and training is equivalent to an accredited advanced practice MSc. Practitioners undertaking this route are not eligible for NHS England training grants, which are specifically designed to support advanced practice trainees to complete MSc (level 7) advanced practice programmes. More information about this route can be found here https://advanced-practice.hee.nhs.uk/our-work/eportfolio-route/.
Q 4.5 How are advanced practice roles funded?
Answer: Advanced practice job roles are not funded by NHSE – East of England. Job roles should be funded from an employing organisation’s existing workforce budgets. In primary care, some qualified advanced practice roles can be funded via the Additional Roles Reimbursement Scheme (ARRS). Visit https://www.england.nhs.uk/gp/expanding-our-workforce/ for more information about the ARRS.
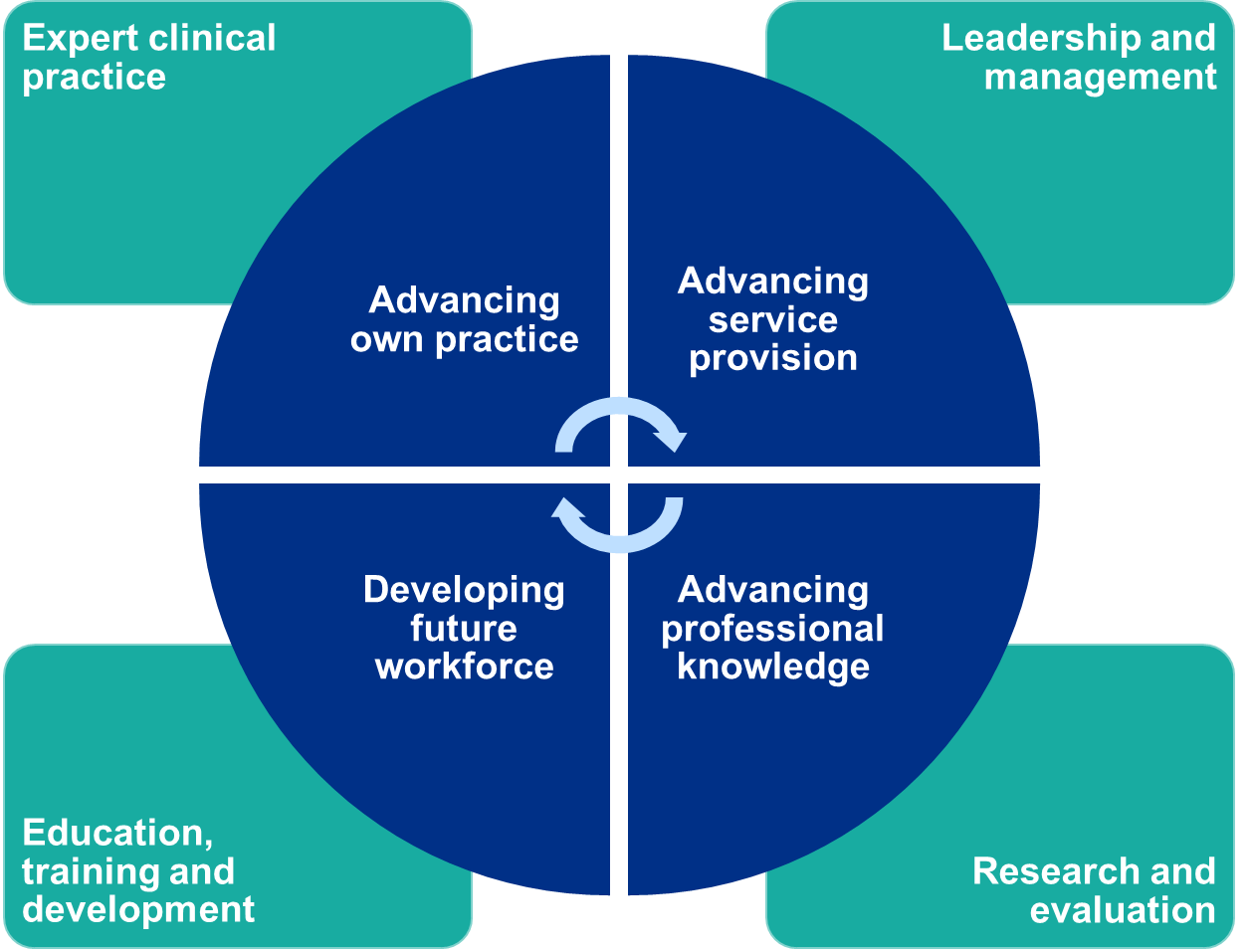
Q 4.6 What stages are involved in advanced practice training funding?
Answer: There are four core stages involved in the process of NHSE funding advanced practice training:
- Organisations apply for funding based on indicative need (see Applying for funding)
- NHSE communicates funding intentions to organisations (see Confirming funding)
- Organisations confirm to NHSE actual funding need (see answer to Q 3.5)
- NHSE confirms and releases funding to organisations (see Payment of funding)
These stages are illustrated in diagram 2 on the right with approximated timelines.
Diagram 2 – Funding stages
*Please see answer to Q 4.14 for further information
** Please see Q 4.16 for further information
Applying for funding
Please note: For further questions about applying for funding which are not answered here, please see the NHSE East of England advanced practice training funding FAQ document which can be found here.
Q 4.7 How is funding applied for?
Answer: Applications for advanced practice training funding are submitted to the Faculty via a specific Excel template.
Q 4.8 When can funding be applied for?
Answer: The window to submit funding applications opens in February and closes in March of the same year. This will occur yearly.
Q 4.9 Who can submit funding applications?
Answer: In secondary care, an organisational advanced practice lead should be the only person within the organisation putting forward applications for NHSE advanced practice training funding. Within primary care, the local primary care training hub lead submits funding applications on behalf of primary care organisations within their catchment.
Direct applications from trainees, line managers, GP practice managers or department leads will not be accepted by the Faculty. To express an interest, contact your organisation’s/primary care training hub’s advanced practice lead. If you are unsure of who your organisational advanced practice lead or primary care training hub is please contact england.eoeapfaculty@nhs.net.
Confirmation of funding
Q 4.10 How does NHSE confirm a funding application has been accepted?
Answer: The organisation or primary care training hub will receive an email from england.eoeapfaculty@nhs.net which will contain:
- An electronic letter outlining the conditions of funding.
- An Excel workbook which contains data on what funding has been indicatively agreed.
Q 4.11 When does NHSE confirm a funding application has been accepted?
Answer: Indicative funding for new advanced practice funding requests is usually confirmed in May each year.
Q 4.12 Is funding guaranteed after NHSE accepts a funding application?
Answer: No. When the Faculty agree indicative funding for new advanced practice trainees, the funding stated is conditional. Organisations or primary care training hub must provide assurance to the Faculty that a trainee has successfully been recruited and will be starting their course on the date indicated in the application. To obtain this assurance, the Faculty require organisations and primary care training hubs to complete a funding utilisation return (see answer to Q 4.13) before funding will start to be paid to organisations and/or education providers.
Q 4.13 What is a funding utilisation return and why must it be completed?
Answer: Organisations and training hubs are required to complete a funding utilisation return before NHSE – East of England will start payments of funding. The return is made using the same Excel workbook sent from the Faculty to confirm funding (see answer to Q 4.10).
The Faculty requires assurance that a trainee has successfully been recruited and is ready to start their course on the date indicated on the funding application before prior to commencement of funding to organisations and/or education provider
Q 4.14 When must a funding utilisation return be completed?
Answer: This is dependent upon the agreed funding start date. This is outlined in the table below.
Table 4 – Funding utilisation return deadlines
|
Payment start |
Return deadline |
|
Between Apr and Jun |
Last weekday of May |
|
Between Sep and Oct |
Third Friday of Aug |
|
Between Jan and Mar |
Third Friday of Dec |
Payment of funding
Please note: For further questions about payment of funding which are not answered here, please see the NHSE East of England advanced practice training funding FAQ document which can be found here.
Q 4.15 How is funding paid out?
Answer: NHSE – East of England pay advanced practice training funding through invoicing. Organisations and institutions who the Faculty have agreed to provide funding with will receive instructions on how much to invoice for and when to submit invoices in a document called the Education Funding Agreement (see NHSE East of England advanced practice training funding FAQ document here for further information).
Q 4.16 When is funding received?
Answer: Advanced practice funding is usually paid out in monthly instalments and NHSE – East of England will instruct organisations and institutions via the Education Funding Agreement to invoice in this pattern ((see NHSE East of England advanced practice training funding FAQ document here for further information). Once NHSE – East of England receives and approves an invoice for advanced practice training, the payment is made to the organisation or education provider within 3 business days.
Q 4.17 What if a change has occurred that impacts funding?
Answer: It is imperative that the Faculty are informed of any changes that might impact payments for advanced practice training it has agreed to fund. If a change of circumstance happens before a trainee commences training, it is the responsibility of the employing organisation or primary care training hub to inform the Faculty – see answer to Q 4.13 for further instructions. Changes that happen after a trainee has already commenced training must be reported to the Faculty – see Trainee changes and funding for further instructions.
Trainee changes and funding
Please note: For further questions about trainee changes and funding which are not answered here, please see the NHSE East of England advanced practice training funding FAQ document which can be found here.
Q 4.18 What if a trainee withdraws from training?
Answer: The trainee is required to complete and submit a notification of change form to the Faculty as soon as they know they will be withdrawing from the programme. The form must be countersigned by the trainee’s employer. The form can be downloaded from this webpage.
Where a trainee withdraws from a programme, funding that was being paid by NHSE – East of England to the employer or education provider will stop the month after their leave date. Funding will not be reinstated following a withdrawal.
Q 4.19 What if a trainee pauses their training?
Answer: The trainee is required to complete and submit a notification of change form to the Faculty as soon as they know when they will be pausing their programme. The Faculty must know about any pauses to programme, including pauses related to sickness, paternity/maternity leave, career breaks, etc. The form must be countersigned by the trainee’s employer. The form can be downloaded from this webpage. If the Faculty is made aware of a pause without receiving a completed notification of change form, it will contact the trainee to formally request a form is completed. The trainee will have 1 month from the date the Faculty made the request to complete the form, otherwise funding that was being paid by NHSE – East of England to their employer will stop.
Where a trainee pauses programme, funding that was being paid by NHSE – East of England to the employer or education provider will stop the month after their pause date. Funding will be reinstated the month after their return date and the payment end date will be extended to account for the number of months payments missed due to the pause.
For the Faculty to pause funding, a return date (estimated or known) must be provided at the point of notification. In cases where a return date is unknown, funding will stop and the employer must reapply to the Faculty for funding when the trainee returns to programme.
The Faculty will agree to pause funding for up to 1 year. Pauses to training over 1 year must be reviewed by the Faculty on a case-by-case basis. The Faculty will not agree to pause funding for 2 years or more. Where this occurs, funding will stop and the employer must reapply to the Faculty for funding when the trainee returns to programme.
Where a trainee has had long or numerous pauses during their programme, it is the joint responsibility of the employer and the education provider to determine whether the trainee has acquired sufficient workplace training to successfully complete the programme. In such cases it may be beneficial, or necessary, for the employer, education provider and trainee to create a tripartite action plan to ensure the required competencies are achieved before an award is issued.
Q 4.20 What if a trainee changes employer within region during training?
Answer: The trainee is required to complete and submit a notification of change form to the Faculty as soon as they know when they will be moving to their new employer. The form must be countersigned by the trainee’s current and new employer. The form can be downloaded from this webpage. If the Faculty is made aware of a change of employer without receiving a completed notification of change form, the trainee will be contacted to formally request a form is completed. The trainee will have 1 month from the date the Faculty made the request to complete the form, otherwise funding that was being paid by NHSE – East of England to their employer will stop.
It is not guaranteed that NHS England funding will transfer with the trainee. Each notification of change form will be reviewed on a case-by-case basis.
Where a trainee moves to another employer within the East of England (and where the new employer is eligible to receive funding for advanced practice training, see answer to Q 4.4), funding will stop being paid to the former employer and start being paid to the new employer the month after their contract end date. If funding was being paid to the education provider instead of the employer, the funding will continue to be paid to the education provider. See answer to Q 4.21 for advice on trainees moving to employers outside of the east of England.
Where trainees are moving into an area of practice (as part of their change of employer) different from the area their existing education, training and experience is in, this must be indicated on the notification of change form. In such cases, the Faculty will not move NHS England funding to the new employer until it has received tripartite assurance from the trainee, the new employer and the education provider that the trainee remains eligible to complete the advanced practice programme. The Faculty will require completion of a tripartite learning needs analysis and learning plan to address any gaps identified in training and experience required to meet the competencies and capabilities of the new area of practice.
Q 4.21 What if a trainee changes to an employer outside of region during training?
Answer: The trainee is required to complete and submit a notification of change form to the Faculty as soon as they know when they will be moving to their new employer. The form must be countersigned by the trainee’s current and new employer. The form can be downloaded from this webpage. The Faculty will share the completed form with the NHSE Regional Faculty for Advancing Practice responsible for trainee’s new region.
Where a trainee moves to another employer outside the East of England, funding from NHSE – East of England will stop the month after the contract end date at their current employer. There is no guarantee that NHS England funding will continue after this date; currently each NHSE region’s funding rules differ for advanced practice training and the NHSE Regional Faculty for Advancing Practice within the trainee’s new region will decide whether the trainee and their new employer are eligible for continued funding.
Q 4.22 What if a trainee delays the start of their training?
Answer: Answer: If a trainee needs to delay the start of their training programme the trainee is required to inform their employer as soon as possible. The employer must inform the Faculty of this change by completing the utilisation return (see answer to Q 4.13 for further instructions). A notification of change form is not needed in cases where a trainee delays the start of their programme.
Q 4.23 What if a trainee moves to a different education provider during training?
Answer: The trainee is required to complete and submit a notification of change form to the Faculty as soon as they know when they will be moving to their new education provider. The form must be countersigned by the trainee’s current and new employer. The form can be downloaded from this webpage. If the Faculty is made aware of a change of education provide without receiving a completed notification of change form, it will contact the trainee to formally request a form is completed. The trainee will have 1 month from the date the Faculty made the request to complete the form, otherwise funding that was being paid by NHSE – East of England to their employer will stop.
It is not guaranteed that NHSE funding will transfer to the new education provider. Each notification of change form will be reviewed on a case-by-case basis. If a trainee moves to a new advanced practice programme that is ineligible for NHSE – East of England’s funding (see answer to Q 4.4), funding will stop the month after the trainee moves to the new programme and funding will not be reinstated.
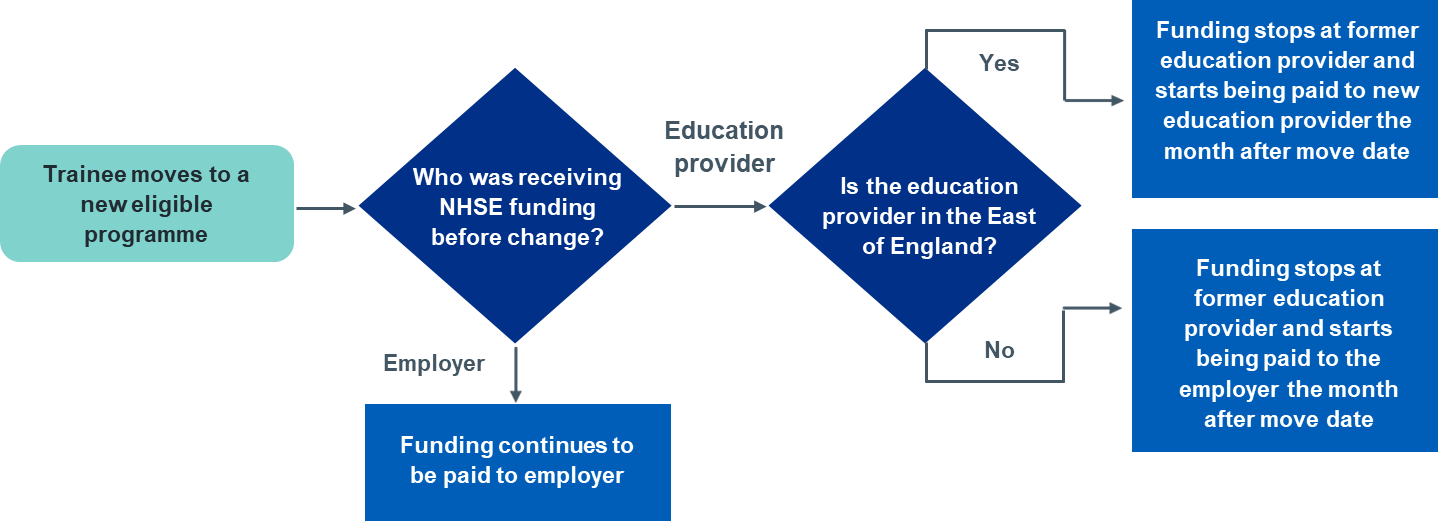
If the trainee moves to an eligible programme, funding will continue after the move date but who is being paid may change depending on the specific scenario. See diagram below for further information. If a new education provider does not recognise the module credits completed at the previous university and requires the trainee to repeat or complete additional modules, NHSE will not provide additional funding above what has already been agreed.
Funding payment changes when a trainee moves university
Trainee monitoring and the impact on funding
Please note: For further questions about trainee changes and its impact on funding which are not answered here, please see the NHSE East of England advanced practice training funding FAQ document which can be found here.
Q 4.24 What is the trainee monitoring survey and how is the data utilised?
Answer: This is an online survey that the Faculty sends directly to all NHSE funded trainees on advanced practice programmes. The purpose of the survey is to monitor the progression of trainees to ensure that funding payments reflect actual trainee activity. The survey also collects demographic data about trainees so that NHSE can monitor the level of equality, diversity and inclusivity of the advanced practice trainees it is funding.
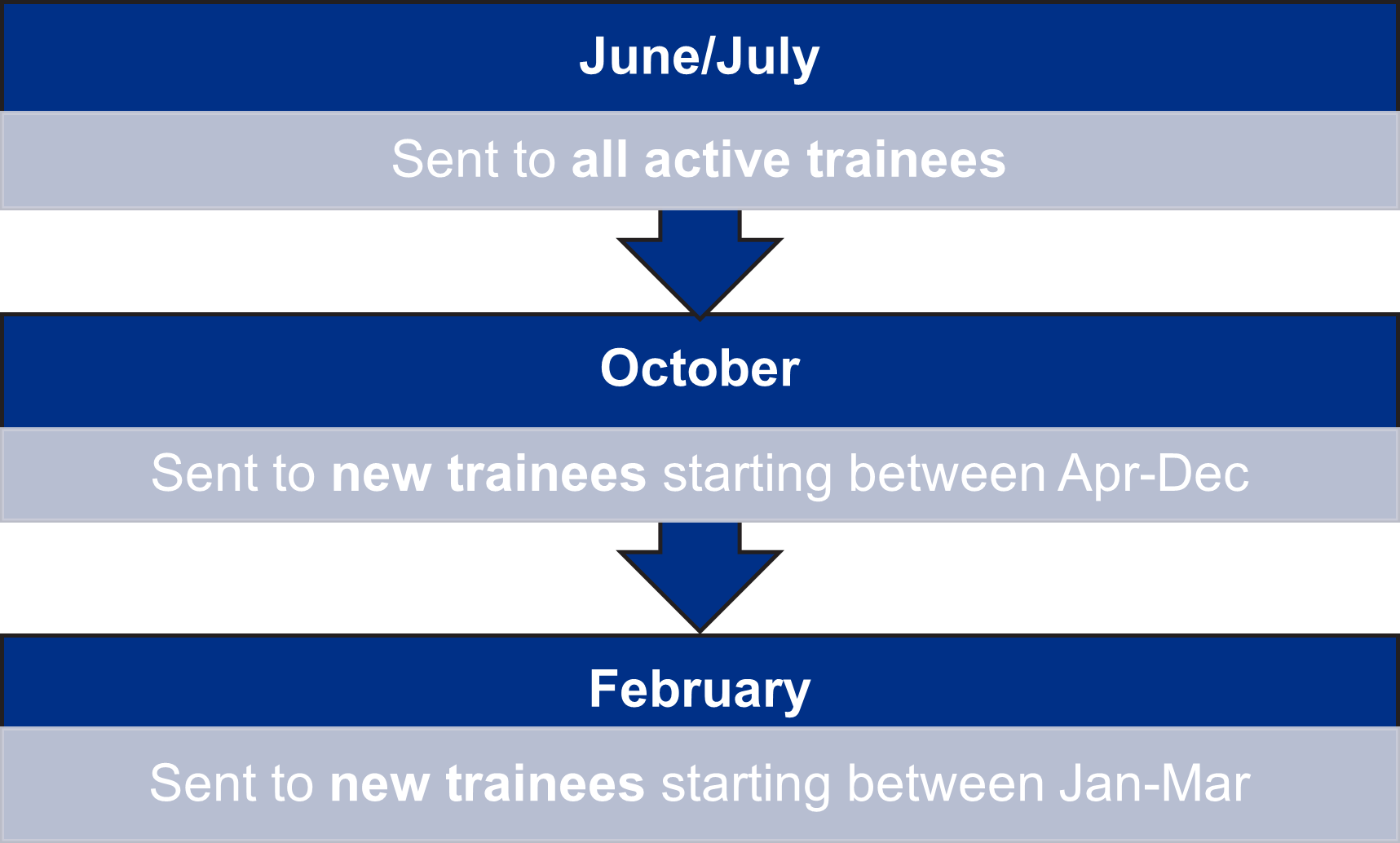
Q 4.25 When is the trainee monitoring survey sent?
Answer: The exact date the survey is sent changes annually, but the month remains the same. The survey is first sent when a trainee starts their programme, and sent subsequently each year whilst they are active students. See diagram for further information.
Timeline of when trainee monitoring survey
Q 4.26 When does the trainee monitoring survey close?
Answer: Each time the survey is sent (see answer to Q 4.25) trainees will be given 6 weeks to complete the survey. The survey takes on average 10 minutes to complete. If the survey is not completed by the trainee within the outlined timeframe NHS England funding will cease.
Apprenticeship funding
Q 4.27 What is the apprenticeship mitigation fund and how is it accessed?
Answer: Prior to January 2026, employers accessed the apprenticeship levy to pay for training costs for staff completing advanced practice degree apprenticeships. As of January 2026, the Department of Education removed access for several level 7 apprenticeships (including advanced practice programmes) for people aged 22 and older. To mitigate for this, the Department of Education have agreed funding that employers can access to cover the training costs for trainees undertaking level 7 apprenticeship programmes that start between finance years 2026/27, 2027/28 and 2028/29. In the East of England, this funding is managed by the Faculty and can be applied for as part of its existing processes – see “Applying for funding”. The eligibility criteria for this funding mirrors the Faculty’s existing requirements – see answer to Q 4.4. The mitigation funding is in line with historical levy price and will be £12,000 total per trainee to be paid at £4,000 per annum over 3 years.
Q 4.28 Can apprentices receive NHSE funding?
Answer: Yes. NHS England – East of England will fund trainees on advanced practice apprenticeship programmes who meet the funding eligibility criteria (see answer to Q 4.5). Trainees on advanced practice apprenticeship programmes can attract the Faculty’s training grant (see answer to Q 4.1) in addition to the Department of Education apprenticeship mitigation fund (see answer to Q. 4.27).

Q 5.1 Which education providers in the East of England offer MSc advanced practice programmes?
Answer: A list of education providers offering MSc Advanced Practice programmes that NHSE-East of England will provide funding for can be found in Appendix 3.
Q 5.2 Can a trainee study at education providers outside of the East of England?
Answer: Please see answer to Q 4.3.
Q 5.3 What is an NHSE accredited advanced practice MSc programme?
Answer: This is an MSc programme certified by NHSE Centre for Advancing Practice that fully integrates all 38 capabilities from the Multi-professional framework for advanced practice in England and meets NHSE’s Standards for Education and Training (2021).
The accreditation process was initiated by NHSE in 2020 to ensure that education providers in England offer a consistent and high–quality level of education for advanced practice trainees.
Completing an NHSE accredited advanced practice programme is one route for practitioners to gain a Digital Badge from NHSE. To find out which programmes have been accredited please visit https://advanced-practice.hee.nhs.uk/our-work/programme-accreditation/. An alternative route for experienced advanced practitioners to gain a Digital Badge is to undertake the NHSE e-Portfolio (supported) Route.
Q 5.4 What is the difference between a direct-entry (non-apprenticeship) and an apprenticeship MSc programme?
Answer: A direct-entry (non-apprenticeship) advanced practice MSc requires a trainee to apply and register directly with the education provider. The trainee should have confirmation from their organisational/primary care training hub advanced practice lead that funding has been approved by NHSE. A trainee is required to complete 180 credits to be awarded an MSc.
An advanced practice degree apprenticeship requires the employing organisation to apply to the education provider. Unlike direct-entry programmes, employing organisations can use their apprenticeship levy (see Apprenticeship funding) to fund the trainee’s tuition costs. Apprenticeships require the employer, trainee and university to sign a commitment statement before the programme starts. A trainee is required to complete 180 credits to be awarded an MSc; this will include a mandatory end-point assessment (EPA). As of January 2026, employers will no longer be able to use the apprenticeship levy to fund the training costs of new advanced practice apprentices who are 22 years old or older (see Apprenticeship funding).
Applying for an MSc programme
Q 5.5 What are the education provider entry requirements for advanced practice programmes?
Answer: Entry requirements for programmes can be found on each education provider website. The links to the webpages for local education providers in East of England can be found in Appendix 3.
Any questions about programme entry requirements, programme content, application process or individual modules should be referred directly to the education provider.
Q 5.6 When should a trainee apply for an advanced practice MSc programme?
Answer: If funding is indicatively agreed by NHSE, the organisational or primary care training hub advanced practice lead should inform the trainee promptly. For direct-entry MSc programmes, the trainee is responsible for successfully applying to an education provider. Apprenticeship programmes will require the employing organisation/training hub to initiate the application.
Each education provider will have different application deadlines. Application deadlines for apprenticeship programmes tend to be shorter than direct-entry programmes. It is therefore important for trainees / employers to apply for a programme promptly after NHSE funding has been agreed.
Trainee support
Q 5.7 What support can a trainee expect from an education provider during training?
Answer: Advanced practice MSc programmes are taught by lecturers and expert clinical practitioners who offer dedicated academic support and guidance. Trainees are allocated a named personal tutor. The education provider also offers comprehensive student support services as well as a dedicated librarian.
A guide for trainee support can be found in Appendix 4.
Trainee change of circumstance
Q 5.8 What happens if a trainee discontinues their programme prior to completion?
Answer: Please see answer to Q 4.18.
Q 5.9 What happens if a trainee leaves the employer that NHSE is currently funding?
Answer: Please see answers to Q 4.20 and Q 4.21.

Appendix 1 – Enhanced and advanced levels of practice
|
Enhanced |
Advanced |
|
· Uses reflection in action to function in unpredictable environment, manages risk defers major decision making · Uses freedom to act but within own scope of practice · Employed in different settings, across professions with a specific body of knowledge · Complex clinical decision making but defers to others for overall plan · Manages a caseload, sometimes providing interventions as part of a dedicated clinical pathway · Will work within national and local protocols where these exist · Post reg/post grad qualifications/CPD occasionally master’s level · Proficient |
· Uses reflection in action extensively, working in an unpredictable environment, manages risk · Has freedom to act and provides professional leadership and supervision in situations that are complex and unpredictable. · Employed in different settings but also has highly developed specific body of knowledge · High level complex clinical decision making, including complete management of episodes of care · Manages defined episodes of clinical care independently, from beginning to end · Will shape the design and delivery of local protocols where these exist · Master’s level · Expert |
Appendix – 2 NHS England funded MSc advanced practice programmes in East of England
University name | Programme name and webpage | Currently accredited? Y/N* |
Anglia Ruskin University | MSc Advanced Practice (Clinical) | Y |
MSc Advanced Practice (Clinical) Degree Apprenticeship | Y | |
University of Bedfordshire | MSc Advanced Clinical Practitioner | Y |
MSc Advanced Clinical Practice Degree Apprenticeship | Y | |
University of East Anglia | MSc Advanced Professional Practice | Y |
MSc Advanced Clinical Practitioner Degree Apprenticeship | Y | |
University of Essex | MSc Advanced Clinical Practice | Y |
MSc Advanced Clinical Practitioner Degree Apprenticeship | Y | |
MSc Advanced Musculoskeletal Assessment and Practice | Y | |
University of Hertfordshire | MSc Advanced Clinical Practice | Y |
MSc Advanced Clinical Practice Degree Apprenticeship | Y | |
University of Suffolk | MSc Advanced Clinical Practice | Y |
MSc Advanced Clinical Practice Degree Apprenticeship | Y |
Appendix 3 – Trainees in need of support
General principles
Trainees requiring support with education provider
There is an expectation for all advanced practice trainees to be proactive in managing their learning journey. This includes acting to manage and resolve problems that may occur during their training programme, with the support of their manager, supervisor, organisational/training hub advanced practice lead, MSc programme lead, and the NHS England – East of England Faculty for Advancing Practice.


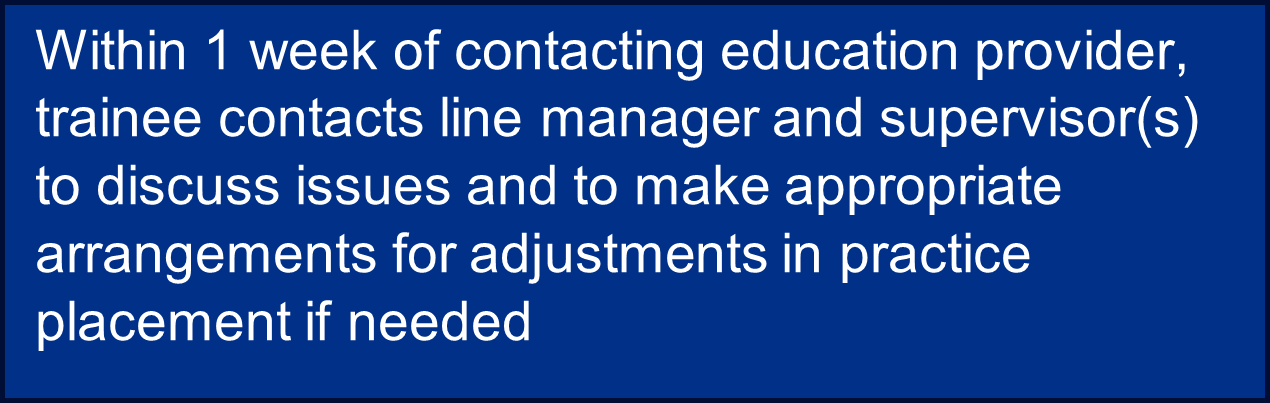
The trainee must report to their line manager and organisation or training hub advanced practice lead immediately if they:
- intend to the leave the programme
- defer on assignments or need to resubmit assignments. These may be education provider assignments or practice placement assignments, portfolios, skills, etc.
- have difficulties in attending required study days, and or are unable to attend
- are considering requesting a deferment, to intermit or pause on their programme
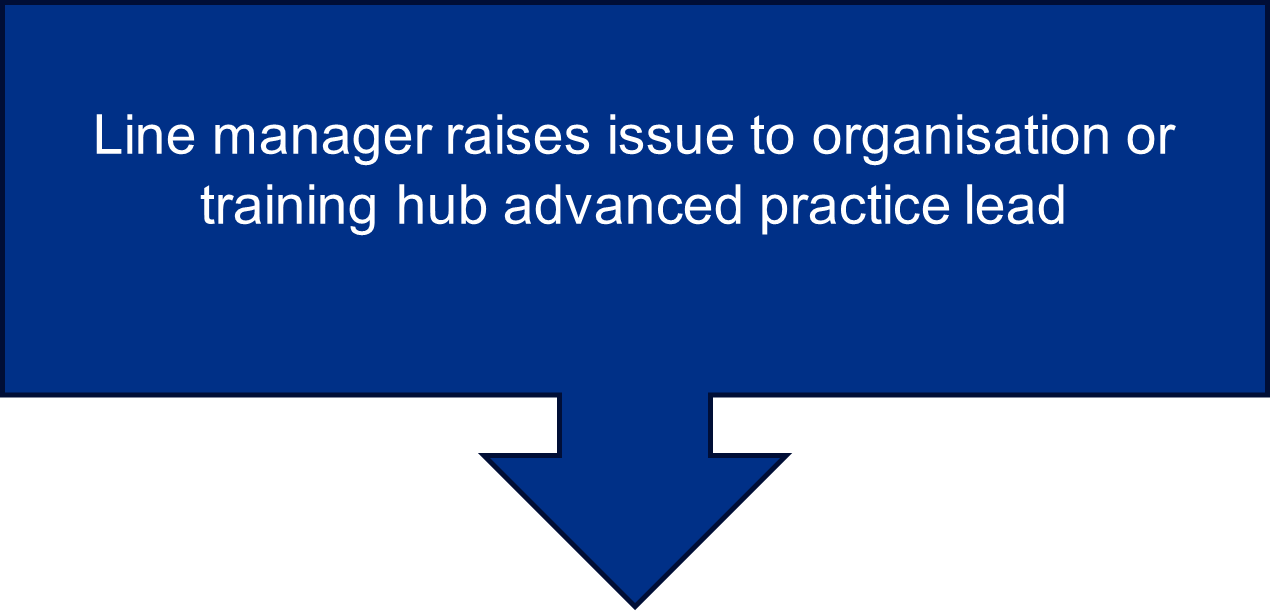
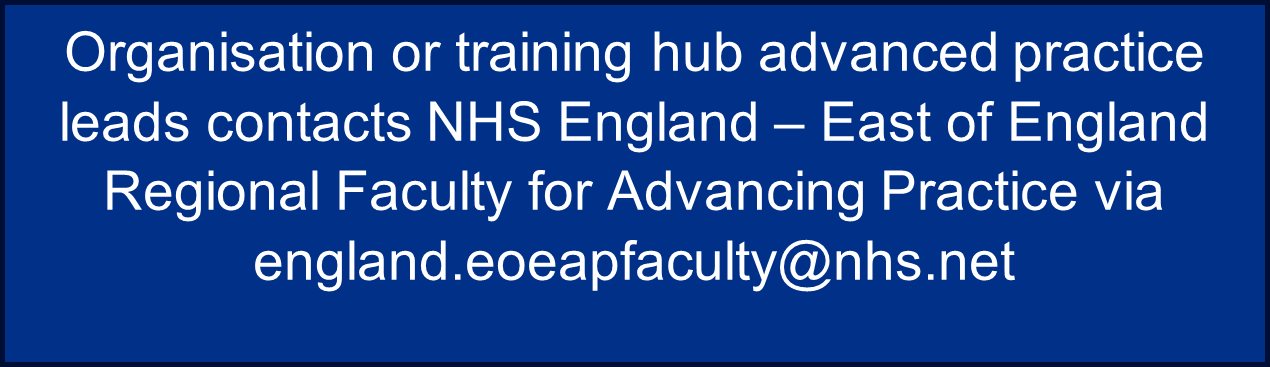
The line manager and advanced practice lead must report any of the above to the NHS England – East of England Faculty for Advancing Practice via england.eoeapfaculty@nhs.net within 7 days of being informed.
Trainees in receipt of NHS England funding who are planning a complete or temporary withdrawal from programme must report this immediately to NHS England via a notification of change form.
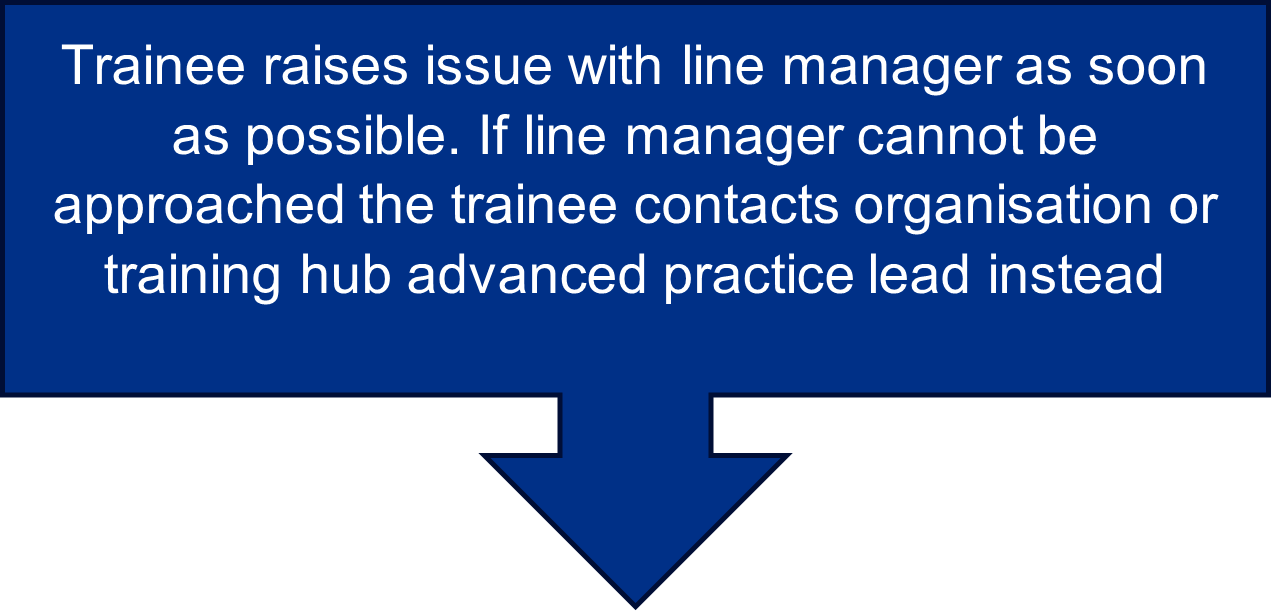
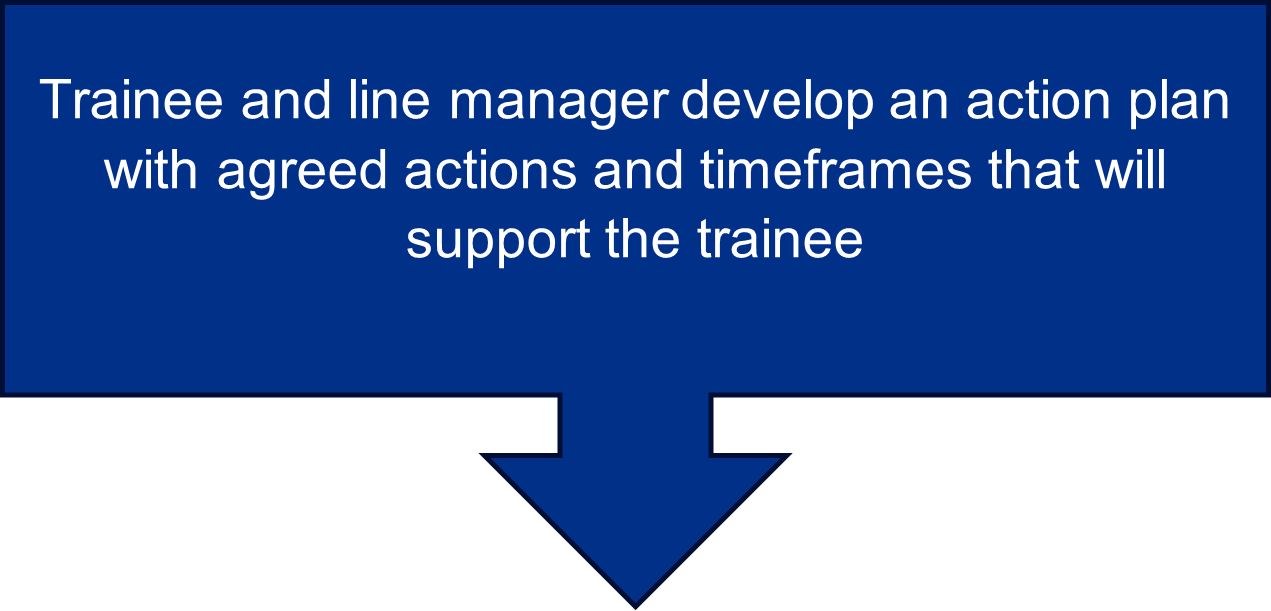
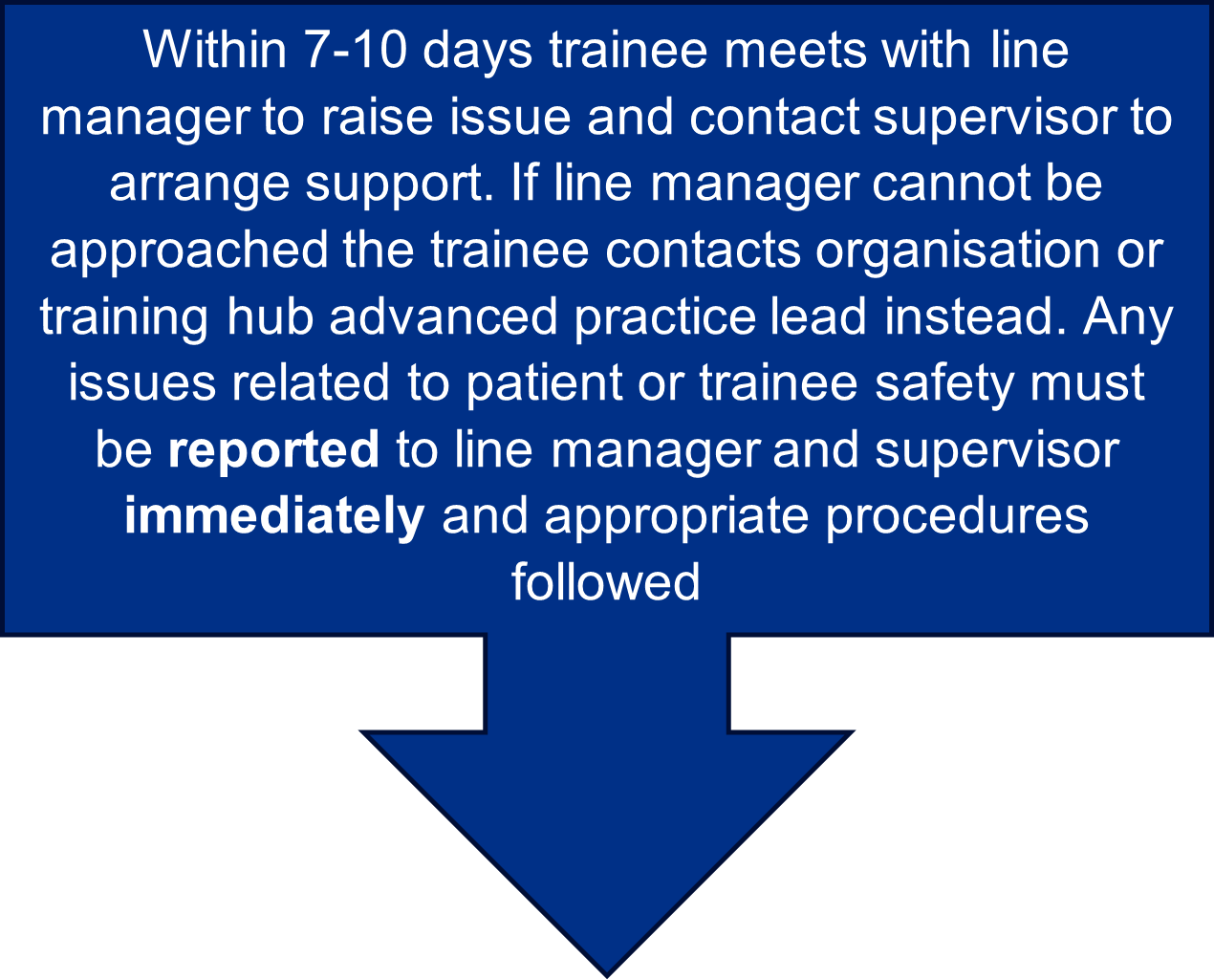
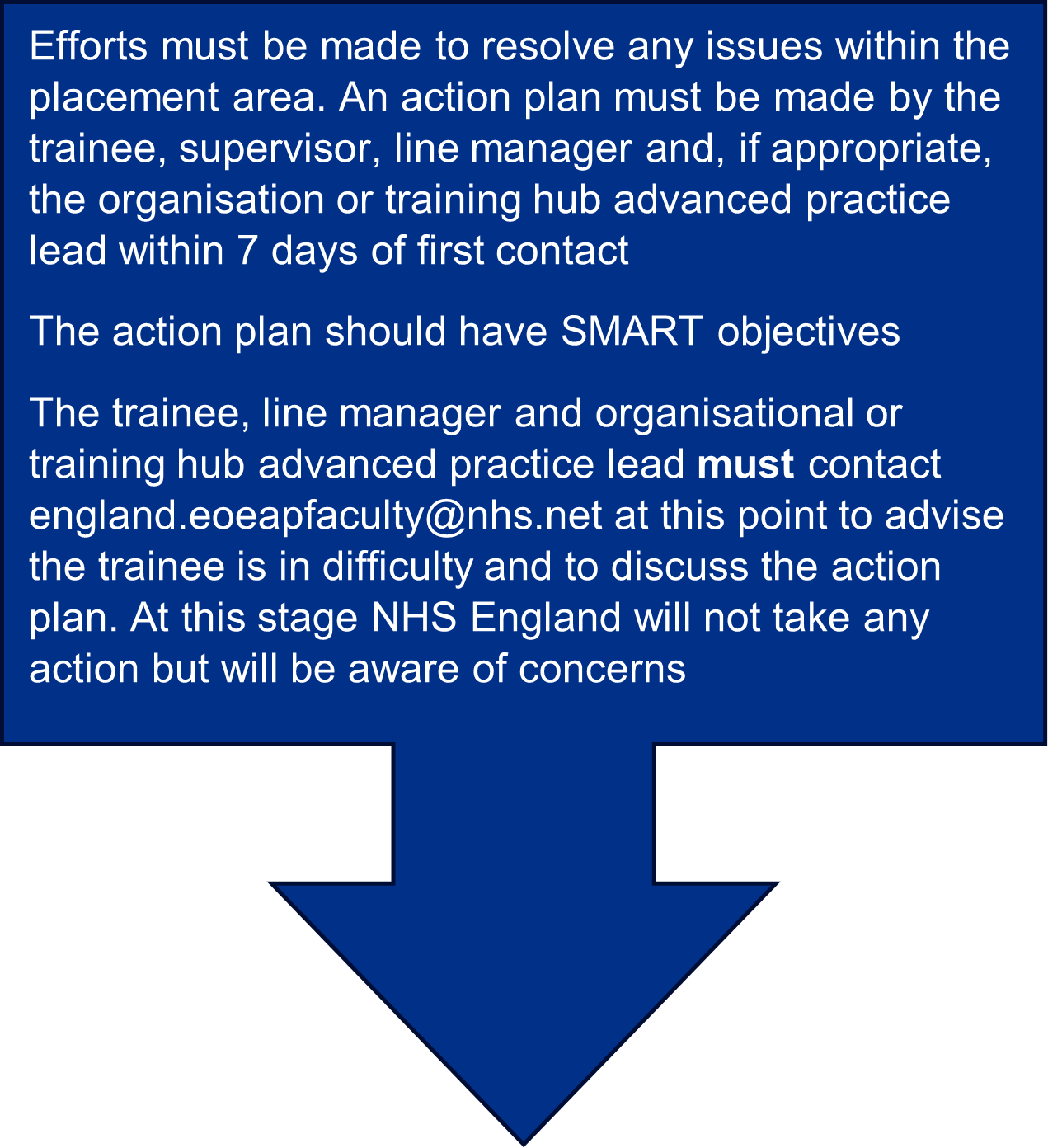
Trainees requiring support in placement areas
There is an expectation for all advanced practice trainees to be proactive in managing their learning journey. This includes acting to manage and resolve problems that may occur during training, with the support of their line manager, supervisor, organisational advanced practice lead, MSc programme lead, and the NHS England – East of England Faculty for Advancing Practice.


Download a full PDF version of this information