This section provides information to support service providers, employers and educators to grow, develop and deploy their advanced practice workforce most effectively.
The Centre for Advancing Practice and the regional faculties
Following the publication of the 1st edition of the framework in 2017, we established the Centre for Advancing Practice and regional Faculties for Advancing Practice to deliver NHS England’s Workforce, Training and Education directorate’s Advancing Practice Programme. Together, the centre and the faculties work to:
- grow and support the development of a multi-professional advanced practice workforce
- promote system-wide understanding of how this workforce can transform services to meet the needs of people, their families, and carers
- help build clear, sustainable career pathways that support workforce development, retention, and transformation
The framework underpins all of this work. The centre:
- establishes and monitors standards for education and training, including in high-priority areas
- accredits advanced practice programmes offered by universities
- supports and recognises the ePortfolio (supported) route
- works to grow and integrate the advanced and consultant practice workforces
Regional faculties in each of the 7 regions in England are well positioned to understand and address their regions’ workforce requirements and this collaborative regional leadership is essential to driving change locally. The faculties:
- provide regional professional leadership, advice, guidance and expertise to NHS England functions, integrated care boards, systems, organisations, and universities on the advancing practice agenda
- support providers and systems in identifying their workforce demand
- commission high-quality education and training
- engage in accreditation processes
- monitor to ensure a standardised quality benchmark is met for those training and entering the workforce as advanced practitioners
- monitor advanced practitioner trainees across each region
- support development of workplace training, supervision, and assessment
- support effective workforce planning that includes advanced and consultant level practice innovations
The continuum of advancing practice
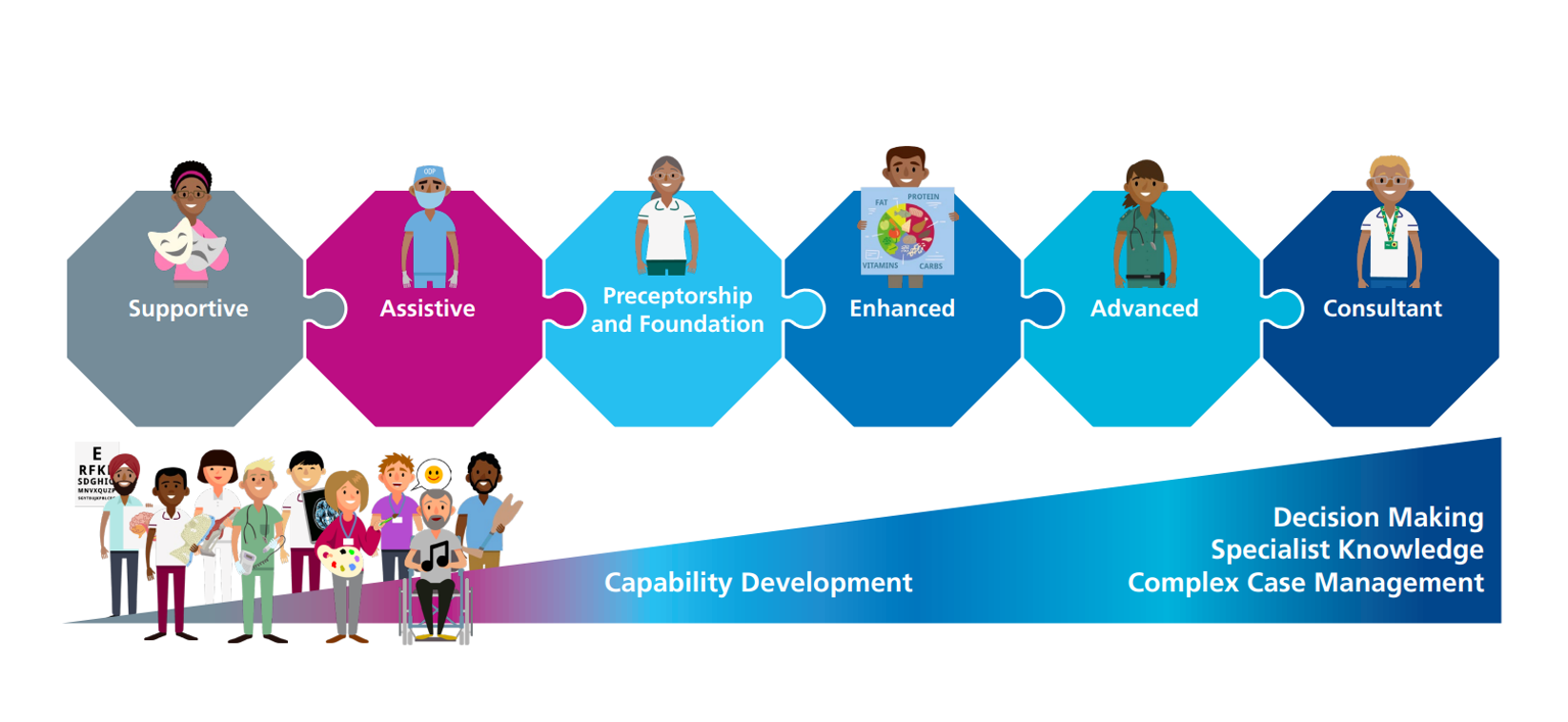
Advanced practice is part of a continuum of advancing practice that spans enhanced, advanced and consultant levels of practice.
Enhanced, advanced and consultant-level practice are steps on a career and workforce development trajectory.
This trajectory starts from qualification and registration as a health and care professional, as practitioners progressively gain the education, training and experience required to develop their knowledge, understanding and skills in roles which have a significant, positive impact on care for people, their families, and carers.
We can define 6 steps in this trajectory of capability development as practitioners become more skilled and experienced in decision making, specialist knowledge and complex case management, with newly qualified registrants starting entry level practice at the preceptorship or foundation stage:
- Supportive
- Assistive
- Preceptorship and foundation
- Enhanced
- Advanced
- Consultant
Enhanced-level practice
This describes the practice of highly experienced, knowledgeable health and care professionals.
Practitioners working at the enhanced level can manage discrete aspects of care within a specific context, which may sometimes encompass whole episodes of care, dependent on the type of care being provided.
In contrast, advanced practitioners frequently manage whole episodes of care from the time a person first presents, through to the end of episodes in a context of complexity, while managing uncertainty and assessing varying levels of risk, holding accountability for decisions they make.
The ‘Principles of Enhanced Level Practice’ (Health Education England, 2023) guidance explains more about enhanced level practice and its contribution to improving services.
Consultant-level practice
Consultant level is an expert level of practice which builds upon advanced practice. Consultant level practitioners are strategic and clinical leaders of healthcare systems.
While advanced practitioners will have the ability to manage and take responsibility for the whole episode of a person’s care, the consultant level practitioner will be able to use their expertise across care pathways and systems and in ways which have maximum impact on practice, services, communities and populations, that add to and sustain workforce capacity and capability.
The NHS England (2023b) Multi-Professional Consultant Level Practice Capability and Impact Framework sets out the capabilities that underpin consultant-level practice. It also indicates how practitioners build on advanced practice to develop into consultant-level roles (NHS England, 2023c).
Advanced practice education and training
This section provides an overview of expectations for the education and training of the advanced practice workforce.
We recognise that education and training in advanced practice has developed over time, and that existing advanced practitioners will have followed different routes into the advanced practice workforce. We recognise and value the continuing contribution of these clinicians to service delivery and care for people, their families, and carers.
Education and training in advanced practice
Below is an overview of education, training, and recognition in advanced practice. The pathway to becoming an advanced practitioner normally involves the following 6 steps. Employer support is essential throughout.
1. Identify
- The employer identifies the need for a prospective advanced practitioner, and the ability of the organisation to fund a future advanced practitioner post.
- They identify the entry requirements and the clinical capabilities for a trainee advanced practitioner position.
2. Entry
- Employer identifies the entry requirements for a trainee advanced practitioner position.
3. Recruit
- In liaison with their regional faculty for advancing practice employers undertake a fair and equitable recruit process and appoint health and care professionals into trainee advanced practitioner positions.
4. Support
- The employer supports the trainee advanced practitioner to complete an accredited master’s programme in advanced practice, which integrates the 4 pillars of practice and associated capabilities across academic and workplace-based supervision, learning and assessment.
- These programmes are normally 3 years in duration. The master’s programme includes both academic preparation and preparation in the workplace.
5. Complete
- On successful completion of the master’s programme, the health and care professional is equipped with the capabilities required to practise at an advanced level.
6. Employ
- The employer employs the health and care professional as an advanced practitioner, continuing to provide appropriate governance, oversight, support and continuing professional development to meet the agreed scope of practice.
Programme accreditation

The Centre accredits programmes in advanced practice which lead to the award of a full post-registration master’s degree. This is normally the award of a Master of Science (MSc) or similar.
Although there is variation in advanced practice itself, by accrediting programmes which prepare health and care professionals for advanced level practice, the Centre can ensure a consistent level of education quality and a consistent level of capability at entry to the advanced practice workforce.
For a programme to become (and remain) accredited, the education provider must demonstrate they meet the Standards for Education and Training and produce graduates who attain the capabilities outlined in this framework.
We embrace diverse programme content to address the unique interests of practitioners and the needs of services. However, all programmes must consistently meet required standards and capabilities, prioritise the needs of individuals, families, and carers, and deliver high-quality academic and clinical preparation for advanced practice.
Accreditation of legacy programmes is possible; these are programmes or iterations of programmes delivered in the recent past, where education providers can satisfy us that they meet our requirements.
We only fund places on advanced practice programmes which hold Centre accreditation or are working towards attaining accreditation.
ePortfolio (supported) route
There will be existing, experienced advanced practitioners who are working in advanced practitioner roles on a regular basis who completed their advanced practice education and training before or soon after the publication of the 1st iteration of this framework in 2017. These practitioners are likely to have completed a programme or older ‘legacy’ programme that the Centre has not accredited.
It is possible for such practitioners to obtain retrospective recognition via the Centre’s ePortfolio (supported) route. Successful applicants for the ePortfolio (supported) route undertake a learning needs analysis with an education provider to understand how far they will be able to demonstrate the framework capabilities.
Applicants complete an electronic portfolio to demonstrate that their educational and experiential learning equivalently meets the framework’s capabilities.
Completing the ePortfolio (supported) route is voluntary for practitioners (and their employers). However, it provides a consistent approach to recognising the experience, knowledge, and skills of existing, experienced advanced practitioners in the workforce.
The ePortfolio (supported) route has been conceived as a quality-assured approach to recognising existing, experienced advanced practitioners, and accordingly is not a training route.
More InformationAdvanced practice area-specific capabilities
The Centre is responsible for developing and implementing standardised multi-professional advanced practice guidance to address high priority, at-scale workforce development needs in discrete speciality areas of practice.
We have previously used the terms ‘credential’ and ‘credentials’ to describe our multi-professional advanced area-specific capabilities documents, comprising standardised, structured units of assessed learning, that are designed to build on this framework to develop advanced level practice capability in a particular clinical area.
These area-specific capabilities are developed to address high priority population and service delivery needs and workforce development intervention in discrete areas of speciality practice.
More InformationThe Centre’s ‘Advanced’ digital badge
Practitioners who have successfully completed either a Centre for Advancing Practice accredited programme or the ePortfolio (supported) route are eligible to download the Centre’s ‘Advanced’ digital badge.
This badge provides clear, standardised evidence that these practitioners have equivalently met the capabilities outlined in the multi-professional framework for advanced practice in England. It verifies that their education and training meet the same rigorous standards, demonstrating educational equivalence to employers, individuals, families and carers.
More information about the Centre’s ‘Advanced’ digital badge and how it benefits practitioners, employers, people, their families and carers is available from the Centre’s digital badge section.
More InformationAdvanced practice governance
Credible governance is essential to the safe, effective, and sustainable employment of practitioners working in advancing practice roles. To support this, the Centre has published the Governance Maturity Matrix, a dynamic tool designed to help organisations assess and optimise their governance of advancing practice.
The matrix enables organisations to self-evaluate their progress across key governance domains, identifying whether they are in the early stages, making substantial progress, or achieving maturity. Its adaptable design ensures relevance across all NHS settings, including acute care, community care, mental health, and primary care.
Importantly, the matrix is not static. Ongoing development will further refine its content, such as integrating consultant-level practice more explicitly and providing supporting commentary to further improve engagement with governance innovations.
This iterative approach ensures the matrix remains a relevant and valuable resource for advancing practice governance in a continually evolving healthcare landscape.
Advanced practice supervision
High quality workplace supervision for healthcare professionals in training is essential for supporting the development of confidence and capability and underpins safety for people, their families and carers, and practitioners.
The trainee advanced practitioner must be supported by multi-professional supervisors; including a nominated co-ordinating education supervisor, who supports practitioners during the period of development. Trainee practitioners should also have access to associate workforce supervisors, who are matched to specified aspects of practitioner development across all 4 pillars of advanced practice.
We have published a comprehensive suite of advanced practice supervision guidance to support service providers, employers and universities in providing effective supervision and assessment of developing advanced practitioners.
Acknowledgements
We would like to thank the following for their contributions to the revision of this framework:
- Inclusivity Group – Centre for Advancing Practice
- Jessie Frost, Chief Sustainability Officer’s Clinical Fellow, NHS England
- Michael Guthrie, (formerly) Policy Lead, Centre for Advancing Practice
- Arnie Puntis, Research and Policy Manager, NHS Race and Health Observatory
- Association of Advanced Practice Educators UK (AAPEUK)
- Regional faculty leads for advancing practice and Centre for Advancing Practice team
- NHS England People’s Advisory Forum

