Midwifery: Capability Framework published November 2022
Introduction
The NHS England (formally Health Education England) Maternity Workforce Strategy (2019) highlighted the complexity and number of services provided in maternity care. To support population health needs there is recognition of the requirement for new roles and possibly new levels of practice within midwifery to support ways of working within the transformation of maternity services. An Advanced Clinical Practice in Midwifery Capabilities Framework has been produced to enable the development of these role in midwifery.
What is Advanced Clinical Practice?
The definition of Advanced Clinical Practice is provided by NHS England.
Advanced Clinical Practice is delivered by experienced, registered health and care practitioners. It is a level of practice characterised by a high degree of autonomy and complex decision making. This is underpinned by a masters level award or equivalent that encompasses the four pillars of clinical practice, leadership and management, education and research, with demonstration of core capabilities and area specific clinical competence.
Advanced Clinical Practice embodies the ability to manage clinical care in partnership with individuals, families and carers. It includes the analysis and synthesis of complex problems across a range of settings, enabling innovative solutions to enhance people’s experience and improve outcomes.
This definition therefore requires that health and care professionals working at the level of advanced practice will exercise decision making in the context of complexity, uncertainty, and varying levels of risk, holding accountability for decisions made.
The Centre for Advancing Practice supports individuals and organisations using the Multi-professional framework for Advanced Clinical Practice in England (2017) It provides standardisation for programmes of education that support underpinning to advanced clinical practitioners. It also supports those already practising at higher levels to gain recognition through a portfolio route. The framework is based on four pillars that uphold this level of practice (Figure 1).
The framework describes requirements for those claiming Advanced Clinical Practice status as follows:
‘…health and care professionals working at the level of Advanced Clinical Practice should have developed and can evidence the underpinning competencies applicable to the specialty or subject area, i.e. the knowledge, skills and behaviours relevant to the health and care professional’s setting and job role.
The core capabilities across the four pillars – clinical practice, leadership and management, education and research are then applied to these specialist competencies. These may be manifested/demonstrated in different ways depending on the profession, role, population group, setting and sector in which an individual is practising’.
Although developed to demonstrate the level of practice across multiple professions there has been a movement in several disciplines to create further specific capabilities or clinical competencies. Before considering Advanced Clinical Practice in midwifery, it is important that there is clarity about the role of the midwife and how the proficiencies described at the point of registration can be developed through education and training from registered practitioner, through enhanced level to advanced level and then to consultant level practice to ensure career development.
Findings from the Deep Dive Report into Advanced Clinical Practice in Midwifery
A literature review conducted by the University of East Anglia demonstrated there is limited international consensus on Advanced Clinical Practice in Midwifery (Goemeas 2018) and international literature specific to midwifery is sparse (Casey 2017) because the number of midwives who hold advanced practice in the title of their posts is small. Whilst there appears to be a range of clinical specialist roles in the profession. In Australia there was recognition of advanced midwifery practice in 2009 but the Australian College of Midwives stated that advanced practice was an illustration of midwives working within their full scope of practice and not advanced skill level (Smith et al 2010). However, in 2009 the Royal College of Midwives recognised advanced capabilities when it described 4 areas of responsibility for consultant midwives i.e.: expert clinical practice; clinical and professional leadership; research and education; practice and service development. There is potential for confusion created by role titles including specialist midwife, advanced practice midwife or advanced midwife practitioner and consultant midwife and it is important to remember that advanced practice is a level of expertise rather than a role title.
The Irish studies (Begley et al 2013; O’Connor et al, 2018; Casey et al 2019) described mainly roles held by clinical specialist midwives and these roles incorporated many elements of advanced practice including facilitating education for multi-disciplinary teams, co-ordinating research, leadership of care including complex care as well as publishing and dissemination of research and evaluative studies. These studies collectively formed a body of evidence which informed the development of the standards for advanced practice in Midwifery by National Board for Nursing and Midwifery, Ireland (NMBI 2018). Casey et al (2017) conducted a rapid review of 86 papers which mainly focused on Advanced Clinical Practice in nursing, with only limited evidence of midwifery advanced or specialist roles drawn from earlier work by Begley and colleagues in Dublin. Advanced Clinical Practice roles in midwifery in Ireland now span primary care, and acute settings. The competencies described by the NMBI include the following broad areas: using advanced assessment and intervention strategies; using research when making clinical decisions; analysing complex interactions; guiding decision-making; and developing client focused care. There is recognition even within the standards document that governance, leadership and infrastructure are needed to implement and support the roles in organisations. The need for an educational pathway with support from higher education and employers is also highlighted to ensure sustainability.
The Deep Dive report into midwifery Advanced Clinical Practice in 2021 identified confusion about how the level of practice might be used in maternity organisations. The confusion limited the access to programmes of education for midwives to complete Advanced Clinical Practice education. The transformation agenda has however created an opportunity for service redesign, and we found that some services were providing opportunities for midwives to practise at this advanced level to provide services to meet local population need. Routes into Advanced Clinical Practice in Midwifery were unclear, however.
The report also included a mapping exercise in which NMC Standards of Proficiency for Midwives were mapped against the Multi-professional framework for Advanced Clinical Practice in England (2017), to test the theory that midwives practise at advanced level from point of registration. (Appendix 1)
The argument that midwives are already working at Advanced Clinical Practice level was captured in the data from HOM/DOMS and consultant midwives within the Deep Dive report. The specialist midwives and advanced clinical practitioners we spoke to were clear that the higher level of practice in their roles required further clinical skills development acquired through a combination of advanced level study and higher-level capabilities in leadership, management, education and research. We conducted an exercise mapping the NMC (2009, 2019) midwifery standards to the Multi-professional framework for Advanced Clinical Practice in England (2017) to identify where the NMC standards might enable practitioners to meet Advanced Clinical Practice levels of practice and where there were gaps. The level of practice and skills described in the proficiencies are designed as the point at which midwives enter the professional register.
The NMC 2009 standards for competence for midwives, states that midwives should be autonomous practitioners and lead care for women experiencing normal childbirth. The 2019 NMC Standards of proficiency for Midwives document provides a very detailed account of the expected role of the midwife based on the Lancet definition of midwifery and framework for quality maternal and newborn care as described earlier. We took account of the following passage from preamble in the 2019 standards, describing the scope of the midwife:
Critical thinking, problem solving, positive role modelling, and leadership development are fundamental components of safe and effective midwifery practice. Midwives play a leading role in enabling effective management and team working, promoting continuous improvement, and encouraging a learning culture. Midwives recognise their own strengths, as well as the strengths of others. They take responsibility for their own continuing professional development and know how they can contribute to others’ development and education, including students and colleagues.
They have the ability to develop in their careers in directions that can include practice, education, research, management, leadership, and policy settings. They continue to develop and refine their knowledge, skills, resourcefulness, flexibility and strength, self-care, critical and strategic thinking, emotional intelligence, and leadership skills throughout their career
This passage indicates clearly that within the scope of midwifery practice there is opportunity for midwives to develop their skills and knowledge in a range of directions. While the midwife is recognised as the ‘lead professional for care and support of women and newborn infants’, the standards suggest that there is room for development and growth across the career span of a midwife. So, the proficiencies therefore act as a baseline and do not, in any way, restrict development. It seems to indicate that development can take place across any or all of the four domains of advanced practice.
The list of proficiencies in the 2019 document is long and detailed, explicating skills and knowledge required at the point of registration. In the mapping exercise we explored in detail the language used to describe the proficiencies when mapping against the Multi-professional framework for Advanced Clinical Practice in England (2017). We have used a Red, Amber, Green approach to indicate where the proficiencies do not match, partially match or match (Table 4). We recognise that this mapping exercise is not an exact science and midwives working in different organisations will have opportunities to use different skills set. We drew on our experience as educators to consider the proficiencies at the point of registration.
Some proficiencies stated the midwife should demonstrate skills whilst others suggested that they need to have knowledge, rather than specific skills. For example, although the 2019 standards suggest that registrants will have knowledge to support prescribing, they will not have the skills to prescribe medicines until they have completed all the requirements in practice supported by evidence. Therefore, although they can give lifestyle advice, and supply some drugs under midwifery exemptions they do not meet the advanced practice level of assessing, diagnosing and prescribing i.e.
Initiate, evaluate and modify a range of interventions which may include prescribing medicines, therapies, lifestyle advice and care.
As a consequence, we rated this as amber in table 4. Indicating that the Advanced Clinical Practice attribute is partially fulfilled by the 2019 proficiencies. It was clear that many of the clinical attributes in the Multi-professional framework for Advanced Clinical Practice in England (2017) could be met by midwives, at least to some extent, particularly those who will in the future graduate with the proficiencies in the latest NMC standards.
Many of the management and leadership, research and education attributes in HEE’s (2017) Multi-professional framework for Advanced Clinical Practice in England will require exposure, experience and education to enable midwives to work at the required level. Following analysis, it seems clear that the Multi-professional framework for Advanced Clinical Practice in England (2017) is suitable for midwives to use in developing the skills and knowledge to reach the Advanced Clinical Practice level within the scope of midwifery.
The mapping exercise (Appendix 1) showed gaps in the proficiency standards when mapped against the the Multi-professional framework for Advanced Clinical Practice in England (2017), demonstrating there was room for growth and development in midwifery careers to reach Advanced Clinical Practice level. The report clearly demonstrated that Advanced Clinical Practice is a level of practice that is beyond that of the qualified midwife at the point of registration. It is not a single definable job role as the roles undertaken by advanced clinical practitioners vary according to the service and population need.
We made recommendations for the development of a career and education pathway to support employers and midwives and this capability framework is the first step in that process. Subsequently University of East Anglia was commissioned to develop a two-stage project with the aim of firstly developing a capability framework for Advanced Clinical Practice in Midwifery and second to produce an education and career pathway framework document for HEIs and Employers. This report details the development and outcomes of the Midwifery Capability Framework for Advanced Clinical Practice in Midwifery.
Preparing the capability framework for Advanced Clinical Practice in Midwifery
The work on developing a capability framework for Advanced Clinical Practice in Midwifery began in January 2022. The team of academic midwives from University of East Anglia was commissioned to develop the capability framework for Advanced Clinical Practice in Midwifery and to follow up with a career and education pathway. The process undertaken to produce the capability framework was as follows, with the key aim to agree a set of capabilities for a midwifery specific Advanced Clinical Practice framework to enable interpretation of the Multi-professional framework for Advanced Clinical Practice in England (2017) through a midwifery prism.
Initiation
- Desktop exercise examining NMC Standards of Proficiency for Midwives (2019), the Multi-professional framework for Advanced Clinical Practice in England (2017) discipline specific advance practice frameworks e.g. Primary Care, Mental health
- Use of the quality framework for maternal and newborn health (Renfrew, McFadden, Bastos, Campbell et al. 2014) to assist with incorporating midwifery specific language into capability statements
Stage 1:
Members of the national steering group for Advanced Clinical Practice in Midwifery and Health Education England (now NHS England) Task and Finish groups for Midwifery capabilities were invited to take part in workshops. They were able to invite others with relevant expertise such as employers and experienced Advanced Clinical Practitioners in Midwifery.
Two workshops were held
Workshop 1 identified, key attributes and values associated with the higher level of practice in midwifery. Mentimenter was used for values statements and attributes. This enabled creation of a word cloud.
The project team created a Padlet as an online tool for capturing thoughts and discussion using the four pillars of advanced practice and the quality framework for maternal and newborn health to act as guide. Participants inputted ideas during and after workshops.
Stage 2:
- Data analysis was conducted by UEA project team
- Capability statements were created and presented to Health Education England (now NHS England) task and finish group
- Further discussion in the task and finish group related to the NMC proficiencies and it became clear that we needed to enable users of the capability statements to understand if and how the statements related to or built upon the Standards of Proficiency for Midwives.
- A framework to explain the relationship to NMC proficiencies for midwives and the Multi-professional framework for Advanced Clinical Practice in England (2017) was created
- The final statement list was tested with the National steering group for Advanced Clinical Practice in Midwifery, refined and agreed.
Participants in workshop 1 included Advanced Clinical Practitioners, Consultant Midwives, Leaders in Midwifery practice, Nursing and Midwifery Council, Royal College of Midwives, Lead Midwives for Education from Higher education Policy, came together online to discuss the key attributes of Advanced Clinical Practice from a midwifery perspective and to explore the capabilities of a Midwifery Advanced Clinical Practitioner. Service user perspectives were provided by testimonies brought by those working in advanced practice roles.
Values and Attributes

To capture the values and attributes that are associated with an Advanced Clinical Practitioner in Midwifery a mentimeter was used and all participants provided 3 words or phrases. The data provided is shown within Figure 2.
It is clear from the values and attributes provided, that those working as an advanced clinical practitioner in midwifery will be required to work across all 4 framework pillars provided by the Multi-professional framework for Advanced Clinical Practice in England (2017), i.e. Clinical Practice, Leadership and Management, Education and Research (Figure 4).
Throughout the workshops we used the Multi-professional framework for Advanced Clinical Practice in England (2017) and the NMC standards of Proficiency for Midwives as a guide to aid discussions. It was important to keep in mind the proficiencies expected of all midwives and consider how these might develop with education, experience, skills training and leadership mentoring. The workshops took place as online discussion forums in which debate and discourse was encouraged to reach a point of consensus through repeated meetings. However not all meetings included the same attendees therefore there were points of discussion which were revisited on a number of occasions.
The UEA project team devised a Padlet to record the workshop participant’s comments, thoughts and opinions by linking the Multi-professional framework for Advanced Clinical Practice in England (2017) capabilities to the framework for maternal and newborn care (Renfrew et al 2014), thus allowing midwifery language, values and priorities to be incorporated into the developing midwifery Advanced Clinical Practice capabilities. During these discussions attention was regularly brought back to the Standards of Proficiency for Midwives NMC (2019). It was recognised that the Advanced Clinical Practice capabilities would originate from the NMC proficiencies building upon them to ensure midwives working at advanced level are demonstrating capabilities complementing the multi-professional framework with a clear focus on the population they serve.
[Midwives] have the ability to develop in their careers in directions that can include practice, education, research, management, leadership, and policy settings. They continue to develop and refine their knowledge, skills, resourcefulness, flexibility and strength, self-care, critical and strategic thinking, emotional intelligence, and leadership skills throughout their career (NMC 2019 p4).
The three requisites for Advanced Clinical Practice in Midwifery are shown in Figure 3:
- Registration as a midwife on the NMC Register
- The generic capabilities identified across the four pillars of Advanced Clinical Practice, as defined in the Multi-professional framework for Advanced Clinical Practice in England (2017) namely Clinical, leadership and management, education, research.
- The Advanced Clinical Practice in Midwifery core capabilities
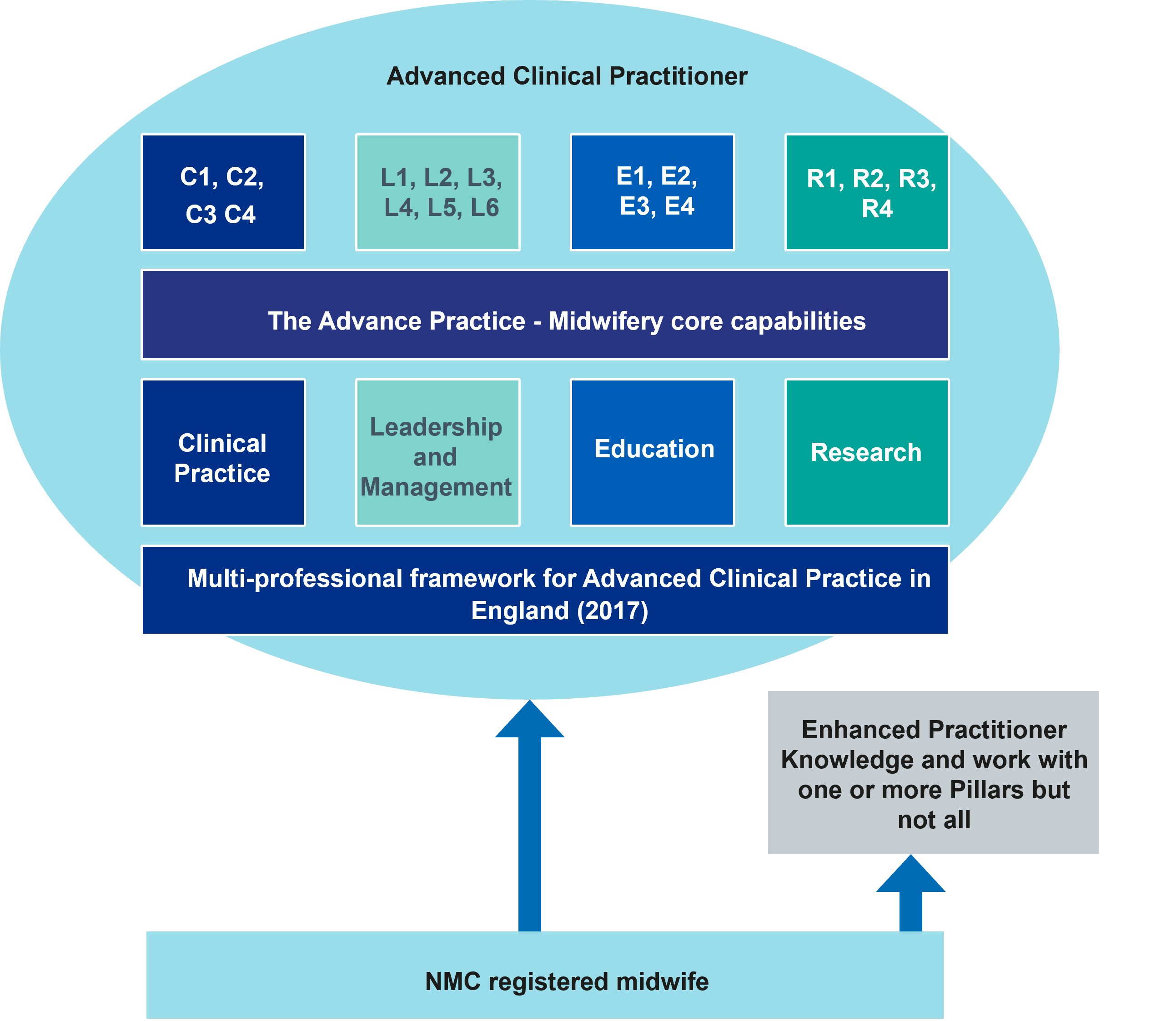
The following capability statements show, where applicable, the origins of the skills and knowledge within the NMC standards of Proficiency for Midwives. The Advanced Clinical Practice in Midwifery Core Capabilities will be reached through formal education and training in the clinical environment supported by a structured programme and mentorship building on this baseline proficiency standard. New levels of skill and competence in decision making will be demonstrated and assessed as part of a programme of development ensuring that all four pillars of advanced practice form part of the performance of the Advanced Clinical Practitioner in Midwifery.
Advanced Clinical Practice in Midwifery Core Capabilities
Having developed expanded levels of knowledge and skills that enable midwives to perform at a higher level of practice. Advanced Clinical Practitioners in Midwifery will demonstrate the following midwifery specific capabilities within their scope of practice and professional registration.
Clinical Practice
C1. Assess, diagnose, manage and support pregnancy and birth in women and people with medical and social complexity including exercising advocacy and expert judgement when working with uncertainty
NMC proficiency origins: 1.6; 3.23; 4.6; 4.8; 5.19; 6.56; 6.57; 6.60; 6.69; 6.70
C2. Practise shared decision making in partnership with medical colleagues, senior clinicians, women, and their families using broadened critical understanding and expert knowledge.
NMC proficiency origins: 3.25; 6.17; 6.22; 6.45; 6.51; 6.72
C3. Synthesise strands of knowledge to provide comprehensive holistic care related to pregnancy and the life course.
NMC proficiency origins: 4.2; 6.20
C4. Demonstrate autonomy and authority to complete episodes of complex maternity care, prescribing where necessary.
NMC proficiency origins: 3.19; 4.3
Leadership and Management
L1. Demonstrate high level communication skills including to navigate difficult conversations with colleagues and service partners and to advocate for safe and effective care delivery (including, where appropriate to negotiate funding and additional resources)
NMC proficiency origins: 1.15; 4.9; 6.1
L2. Ability to respond to and negotiate evidence-based priority areas of maternity care
NMC proficiency origins: 6.83; 6.84
L3. Embed organisational learning from practice in the local maternity and neonatal system, leading on shared responsibility for learning within a specific area of service
NMC proficiency origins: 5.8; 6.86.5; 6.89.2
L4. Use in-depth knowledge of maternity population needs to lead and drive change and influence local policy for clinical practice which is population focussed, avoids health bias, and considers issues related to equality, inclusivity and diversity.
NMC proficiency origins: 1.9; 1.17.1; 3.2; 5.11
L5. Role model midwifery leadership, resilience, and determination in managing situations that are unfamiliar, complex or unpredictable and seek to build confidence in others caring for the childbearing population.
NMC proficiency origins: 1.25; 5.14; 5.15; 5.20
L6. Possess the agency, knowledge and skillset to break down organisational and cultural barriers and provide collegiate approaches to transparent care planning and support of individual women and birthing people.
NMC proficiency origins: 1.22
Education
E1. Seek out and foster networks of Advanced Clinical Practice in an organisation/ system to learn lessons and share knowledge for best practice across disciplines.
NMC proficiency origins: Not applicable
E2. Use clinical expertise to influence the training and education agenda of the maternity workforce within organisations/systems.
NMC proficiency origins: Not applicable
E3. Role model and facilitate reciprocal multi-professional and multidisciplinary team learning alongside colleagues in women’s and children’s health.
NMC proficiency origins: 5.8
E4. Support midwifery succession planning and career development through role modelling and championing innovative, groundbreaking practice.
NMC proficiency origins: 5.18
Research
R1. Identify organisational need and use quality improvement methodology including audit and evaluation to facilitate co-production, design, and advancement of maternity service
NMC proficiency origins: 5.1; 5.3; 6.83
R2. Identify and participate in networks of aspiring research active clinicians in an organisation/system to inform service change across disciplines that informs maternity care.
NMC proficiency origins: Not applicable
R3. Role model active participation in research and the ability to professionally challenge from strong evidence informed position to advance maternity care.
NMC proficiency origins: 1.4; 5.17; 5.16; 6.3
R4. Ensure the complex needs of the maternity population are met by the service through conduct of evaluation and research.
NMC proficiency origins: 1.5; 3.2
These core capabilities for Advanced Clinical Practice in Midwifery, with The Multi-professional framework for Advanced Clinical Practice in England (2017) are recommended as the outcomes for education and portfolio assessments of midwifery advanced practice. They should be used to develop education programmes and to plan assessments. through their integration within the ‘generic’ requirements of advanced practice
Considerations for employers
The Multi-professional framework for Advanced Clinical Practice in England (2017) provides guidance for employers on governance of advanced practice roles including the following key aspects.
Managers and clinicians should work together to identify where Advanced Clinical Practice can support pathways of care, having maximum impact. Development of roles which require Advanced Clinical Practice capability must be in response to local population need with a view to improving quality and outcomes of care pathways. Examples of roles that have been developed are contained in the scoping review report. These were created in response to identified need to provide particular care pathways. The need for particular care pathways and roles will vary across organisations and populations.
Roles requiring Advanced Clinical Practice capabilities should have a clear purpose and objective and defined sphere with adequate planned support for the role. In planning workforce managers and clinicians should work together to ensure the supply and succession planning of appropriately skilled individuals. Where some individual practitioners are working to a higher level, other practitioners may require support to increase their levels of skills and knowledge. Discussions with local HEIs should support the workforce planning and ensure education is accessible to enable individuals to progress to advanced practice through clear pathways Advice on education and career planning should also be available to practitioners who have a desire to develop. Development of this kind may support retention of staff in organisations.
Where new roles are implemented, evaluation that includes impact on service user experience and care outcomes will provide valuable evidence of the benefits or otherwise of the roles in care pathways.
Four key principles are outlined in the multi-professional framework that are important considerations for all maternity organisations planning for advanced practice roles in new service development.

Individual practitioners, as registered professionals, continue to hold professional responsibility and accountability for their practice.

Employers recognise and accept potential new responsibilities and greater accountability in relation to governance, and support for these roles and associated level of practice.

Professional support arrangements, which recognise the nature of the role and the responsibilities involved, must be explicit and developed.

Employers must ensure regular review and supervision is carried out by those who are appropriately qualified to do so.
Routes to Advanced Clinical Practice in Midwifery
An important element of any workforce planning needs to be education and career development. There was evidence in the Deep Dive report (HEE 2021) that newly qualified midwives aspired to develop their clinical knowledge and skills, along with research, education and leadership and management capabilities, to work at the level of advanced practice.
Some midwives in specialist clinical roles had developed high levels of capability and knowledge in one medical condition, its support and management, and had clearly gained higher level capability in the clinical pillar but had not accessed education and training to develop the other pillars i.e., Management and Leadership, Research and Education. This level of practice could fit the criteria for enhanced practice[1].
Those already practising at higher level and who hold education at Master’s level as outlined in The Multi-professional framework for Advanced Clinical Practice in England (2017)may be able to gain recognition through the HEE Centre’s ePortfolio (supported) route.
To support employers, educators and individual midwives a framework is being created to support midwifery career development from newly qualified midwife to consultant midwife. The framework will aim to signpost routes and education required for each stage of the journey.
Downloads

The Advanced Clinical Practice in Midwifery Capabilities Framework. This framework aims to help create the new midwifery roles required to meet the health needs of the population. (Full download)
