The research capabilities
The expectation is that all practice-based health and care professionals develop these fundamental research capabilities, relevant to their level of practice.
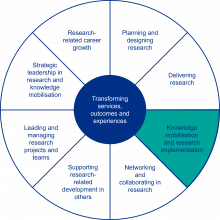
Organisation of the capabilities into eight non-hierarchical, inter-related domains, requires consideration of them as a whole, rather than of individual domains in isolation.
The capabilities presented at each level incorporate and extend those that precede it. Progression to the next level requires first achieving the capabilities outlined at the previous level.
It is recognised that practitioners may possess or choose to develop research capabilities beyond those outlined at a particular level of practice. This might relate to different entry level qualifications. It could apply to those in research delivery leadership roles or actively pursuing a clinical or practitioner academic development pathway.

Multi-professional Practice-based Research Capabilities Framework
The focus of the Research-related career growth domain is on a proactive approach to research-related capabilities development in practice. These capabilities are the foundation for consistently embedding research into the day-to-day practice of all health and care practitioners.
Entry level
- Demonstrate knowledge and understanding of the importance of practitioners’ contributions to developing the knowledge base through active engagement at appropriate levels in audit, service evaluation, quality improvement and research.
- Demonstrate insight into own knowledge creation and research capabilities and developmental needs, and take action to address those needs.
- Constructively question own and others’ practice, identifying opportunities to generate new knowledge and enhance services.
- Develop awareness of local research-related resources and opportunities and how they can be accessed.
Enhanced level
- Proactively discuss own research-related developmental needs with line manager, agreeing realistic objectives and plans to address them.
- Explore and develop plans for own career aspirations integrating practice and research-related activities, making proactive use of local and national resources and opportunities to access guidance and support.
- Link with or build networks to support the development of the capabilities required to actively participate in knowledge creation and mobilisation activities within own role.
Advanced level
- Identify and pursue realistic and achievable research-related career goals, giving specific thought to growing own contributions to the development and application of new knowledge.
- Actively seek out and engage with research-related professional development opportunities, including master’ level education, and other relevant credentials, certificates or qualifications.
- Effectively integrate developing and maturing practice skills and expertise with developing and maturing research skills.
- Plan and pursue opportunities to develop and apply new knowledge to own and others’ practice in structured ways that can be evaluated.
- Contribute to development and delivery of research projects at service level.
Consultant level
- Engage and lead others across the organisation to adopt a supportive culture of research and inquiry that drives service development and improvement.
- Role model commitment to ongoing research-related learning and development in a variety of forms.
- Contribute to and lead research at organisational level and beyond.
- Proactively support others’ critical understanding of differing research methods and analytical approaches.
- Demonstrate the transferability of research-related knowledge, skills and experience between contexts.
The Planning and designing research domain brings together capabilities that underpin the effective critique of research outputs, the evolving evidence base and wider sources of information / data, and the development of robust protocols for individual inquiry and research projects.
Entry level
- Demonstrate broad awareness of knowledge creation processes, including awareness of the basic, underlying principles, concepts and approaches to applied research.
- Appreciate the differences and relationships between audit, service evaluation, quality improvement and research.
- Undertake basic systematic information searches using appropriate tools / databases to identify information and evidence relevant to answering practice-based enquiries.
- Evaluate intervention / treatment plans using recognised and appropriate outcome measures.
- Demonstrate knowledge and understanding of quality improvement systems, processes and methodologies relevant to own discipline, service, department and organisation.
- Recognise the value of, and actively participate in, the systematic gathering and use of qualitative and quantitative data to monitor, evaluate and improve the quality of practice.
- Recognise the importance of working in partnership with people accessing services and wider communities when planning, designing and carrying out research.
Enhanced level
- Demonstrate understanding and application of a range of outcome and quality measures, critiquing and selecting them appropriately for use in inquiry-based projects.
- Confidently undertake systematic information searches using appropriate tools / databases to identify information relevant to addressing practice-based inquiries.
- Identify evidence gaps and contribute to developing practice-based question/s worthy of investigation, including those that could be explored by pre- and post-registration learners undertaking formal academic studies.
- Develop appropriate aims and objectives for inquiry-based projects.
- Demonstrate understanding of the key features of a research protocol and the qualitative and quantitative methodologies commonly used in practice-based research in own discipline.
- Select and apply appropriate approaches to and tools of inquiry to answer practice-based questions, demonstrating understanding of the associated sustainability and ethical considerations.
- Understand and use appropriate technical language in the context of applied research (e.g. research participant rather than patient/client/service user/etc.; data rather than information; statistical significance rather than clinical significance).
- Demonstrate understanding of how to interpret qualitative and quantitative research data and the limitations associated with this, including in relation to own knowledge creation activities.
- Critically analyse the strengths and limitations of quantitative and qualitative studies, including ethical considerations, study design, data analysis and interpretation.
- Analyse and synthesise the findings from small-scale local audit, service evaluation or quality improvement projects, using computing packages and digital technologies as appropriate, and interpreting findings in the light of existing knowledge.
Advanced level
- Undertake advanced information searches using a range of software, databases, resources and techniques, recognising their individual advantages and limitations.
- Critically analyse the evidence base and other relevant information sources to develop and clearly articulate research questions that address the needs and priorities of practice.
- Demonstrate understanding of a range of standard research and quality improvement methodologies and designs and their related ethical considerations.
- With support, design small scale research studies to address issues arising in practice using methodological and analytical approaches that appropriately consider environmental impact and sustainability.
- Work collaboratively with all relevant stakeholders, explicitly embracing and enabling meaningful Public and Patient Involvement / Engagement and co-production, and ensuring a diverse and representative range of contributors and participants.
- Apply understanding of a range of analytical approaches to examine qualitative and quantitative data.
- Make effective use of digital technologies and computing packages relevant to undertaking quality improvement or research projects and the analysis of data.
- Demonstrate insight and critical thinking by clearly identifying own assumptions, and by developing robust arguments that are clear, evidenced and concise.
- Draw on practice and research expertise to contribute constructively to processes for peer review of publications.
- Contribute to the development and submission of research funding applications that reflect the requirements of the target funding body, data protection, information governance, ethical and research governance frameworks and processes.
Consultant level
- Critically appraise and supportively challenge current service provision, proposing and leading research or service improvement within complex and unpredictable contexts.
- Identify trends and changes in the health, wellbeing and needs of a population, including at a national level, to formulate critical questions that justify further research, audit or service evaluation.
- Demonstrate sound understanding of project design, including philosophical underpinnings and theoretical perspectives, and methodological and analytical approaches when planning and leading research and inquiry.
- Work collaboratively to realise the benefits of inter-disciplinary and cross-boundary working in relation to proposed research and inquiry.
- Design research protocols that take account of environmental and sustainability issues and impact at organisational level or beyond.
- Manage complex, incomplete or contradictory data to ensure robust analysis.
- Support and guide the development of research proposals led by others with less experience.
- Contribute to or lead the development and evaluation of the public contributor role in knowledge production.

Research Capabilities Domain 3. Delivering research
Capabilities within the Delivering research domain centre on those related to promoting, supporting, contributing to and engaging in the delivery of research in accordance with the expectations of ethical conduct, robust governance processes and Good Clinical Practice. The capabilities apply to research developed and lead by the individual, as well as research developed and lead by others.
Entry level
- Demonstrate a broad understanding of research ethics and governance processes.
- Understand and apply the principles of information governance, data governance and cyber security to ensure safe and effective use of health, care and other relevant information.
- Understand and apply the requirements for confidentiality regarding research data and patient identifiable data, including the Caldicott principles.
- Demonstrate competent use of relevant digital technologies and devices, including using digital record-keeping tools and changing practice to accommodate new developments, technologies and contexts.
- Engage in research and knowledge creation activities in ways that demonstrate understanding of the impact of environmental sustainability on health and wellbeing.
- Maintain awareness of studies being undertaken in own service, department and organisation, and how to refer people to research delivery teams to discuss possible recruitment to studies.
Enhanced level
- Understand and comply with research ethics and governance processes, data protection and confidentiality requirements in line with Good Clinical Practice, and support less experienced colleagues to do so.
- Promote opportunities for people who access services, their families and carers and wider communities to participate in research being undertaken within own organisation.
- Contribute to the delivery of research projects or clinical trials being undertaken in own service, department or organisation.
- Demonstrate communication skills and strategies that are adapted to meet the needs of different individuals and groups to optimise their engagement in research.
- Participate in audit, service evaluation, quality improvement or projects related to own practice, embracing digital technologies as appropriate.
- Reflect on own experiences of knowledge creation activities and use this information to appraise the work completed and inform future projects and practice.
Advanced level
- Undertake Good Clinical Practice (GCP) training and maintain its currency, effectively applying its principles to safeguard participants and ensure research quality.
- Develop, implement or comply with local research governance processes, demonstrating ethical conduct throughout all aspects of own research and supporting others to do so.
- Apply knowledge and understanding of legal requirements of research (e.g. data protection, mental capacity, safeguarding and human tissue acts, etc.), demonstrating the highest regard for participant’s rights and safety, and data integrity.
- Demonstrate awareness of procedures for reporting concerns about research conduct when breaches of protocol are identified or when fraud / misconduct is suspected.
- Design and deliver audit, service evaluation and quality improvement activity, working with others to develop or benefit from their skills in these areas.
- Contribute to and support the delivery of research designed by others to address issues arising in practice.
- Contribute to the development of study documentation (e.g. participant information leaflet, consent forms, case report forms, data collection, etc.) and related management systems.
- Effectively and sensitively communicate complex information to stakeholders and participants in the context of conducting applied research.
- Critically reflecting on research, evaluation and improvement processes, carrying learning forward to inform how projects are undertaken and managed in future.
Consultant level
- Conduct thorough risk analyses for self, team and others in the context of research and service improvement initiatives, quickly identifying and confidently managing risks.
- Actively engage in and lead delivery of research at or beyond organisational levels to generate new knowledge to inform service design and delivery and enhance the outcomes and experiences of individuals and communities.
- Contribute to delivery of national and international research to generate new knowledge to inform wider system benefits.
- Where relevant to own role and context, demonstrate awareness of licensing authorities and their requirements regarding investigational products and devices.
The Knowledge mobilisation and research implementation domain focuses on capabilities required to make best use of existing evidence, share new knowledge and add to the evidence base in ways that optimise uptake and support the transformation of services, outcomes and experiences.
Entry level
- Engage in evidence-based practice in all aspects of service delivery and provide evidence-based information to enable those accessing services to make informed choices.
- Apply a fundamental understanding of qualitative and quantitative research methods, ethics and governance processes to critically appraise, safely apply and share research findings to inform and promote best practice.
- Demonstrate awareness of the limitations of available evidence, applying appropriate caution regarding how it is used.
- Demonstrate skilful reasoning, problem-solving and critical thinking when applying evidence, drawing on own experience and seeking guidance from more experienced colleagues where appropriate.
- Analyse and reflect on research evidence and other information relevant to own practice to optimise the outcomes and experiences of individuals and communities.
Enhanced level
- Use critically appraised evidence to address problems and questions arising in practice, using own judgement and seeking guidance from more experienced colleagues where appropriate.
- Promote a culture of evidence-based practice using a range of evidence sources including research, scholarship and continuing professional development to inform practice.
- Collaborate with more experienced colleagues to analyse the outcomes of knowledge creation activities, benchmark them against local or regional data where possible, and implement improvements as appropriate.
- Use research evidence to constructively challenge practice that undermines the quality of services or the delivery of expected outcomes for individuals and communities.
- Contribute to the development of local evidence-based guidance.
- Demonstrate understanding of the concepts of authorship and intellectual property, and awareness of the processes involved in peer-reviewed publication.
- Disseminate the findings of knowledge creation activities at a level appropriate to the nature of the work and its outcomes, including through conference presentations.
Advanced level
- Actively champion the central role of evidence-based practice, knowledge mobilisation and implementation science in service developments to improve the outcomes and experiences of individuals and communities.
- Demonstrate critical understanding of the latest evidence relevant to own practice and related fields, appraising and synthesising the outcomes of research, evaluations and audits, effectively integrating it into practice and supporting others to do so.
- Analyse the latest evidence relevant to own practice and related fields to identify any further work required to strengthen evidence for best practice.
- Effectively communicate the relevance of research findings and best practice to colleagues, advocacy groups and the wider community.
- Make identifiable contributions to changes and developments in practice at service level that are informed by research findings.
- Contribute to the development of evidence-based guidelines and policy at service, organisational or national levels.
- Develop outputs from research and quality improvement initiatives that reflect the preferred style and communication method of the target audience/s, working with stakeholders as required to achieve this.
- Disseminates findings from research and quality improvement initiatives through appropriate media and forums, including through publication, to optimise the sharing of knowledge and translation into practice.
- Proactively contribute to knowledge mobilisation practices such as in-service training, communities of practice, and service improvement initiatives, to optimise the timely translation of findings into practice.
- Make effective use of interactive technologies to build a digital presence to support the dissemination of new evidence and own research development and engagement.
Consultant level
- Demonstrate in-depth understanding of the latest evidence within own scope of practice, using and promoting it alongside implementation science frameworks, strategies and tools to improve standards of practice and develop services, organisations and systems.
- Role-model the integration of research and learning to inform practice, including identifying evidence gaps and synthesising knowledge from multiple sources, and support others to do so.
- Lead the development and evaluation of service delivery, informed by research evidence and innovations identified elsewhere and implementation science, sharing the outcomes to improve service delivery beyond the organisation.
- Make identifiable contributions to changes and developments within a profession, organisation or beyond that are informed by research findings.
- Contribute to the development or revision of national or international evidence-based guidance, strategy or policy and their application in practice.
- Generate new knowledge and understanding through research and inquiry, communicating findings to the widest possible audience to benefit service development and delivery and improve the experiences and outcomes of individuals and communities beyond the organisation.
- Lead activities that support knowledge mobilisation, optimising access to new research evidence and innovations, through high-quality publications, professional and public engagement activities and via appropriate media.
- Demonstrate sound understanding of what research impact is, pathways to impact and how impact can be measured and demonstrated.
Research Capabilities Domain 5. Networking and collaborating in research
The capabilities in the Networking and collaborating in research domain centre on realising the benefits of learning with and from others in research, and bringing together stakeholders and differing perspectives and expertise to enhance the quality of research and the building of research capability and capacity.
Entry level
- Recognise the impact of culture and the principles of equality and diversity on practice and knowledge creation activities, and demonstrate anti-racist, anti-discriminatory, inclusive behaviour, responding sensitively to the needs of different individuals and groups.
- Share and extend knowledge and understanding by engaging with peers regarding the outcome of problem solving, audit, service evaluation, quality improvement, research and other developmental activities.
- Engage in and discuss critical appraisals of local data and recently published research findings to support evidence-informed decision making and service development or improvement planning.
- Develop and nurture collaborative partnerships with people accessing services and wider communities to evaluate the effectiveness, and inform the development, of interventions and services.
- Collaborate with interdisciplinary and multi-agency colleagues, service user groups and other stakeholders to promote continuous quality improvement.
Enhanced level
- Role-model an anti-racist, anti-discriminatory approach in all research-related interactions, identifying and appropriately challenging discriminatory behaviours and inequities.
- Demonstrate knowledge of and engagement with local strategies, groups and activities focused on the active involvement and engagement of people who access services and wider communities in research.
- Demonstrate broad and growing awareness of local and national forums and conferences related to practice-based research.
- Facilitate the involvement of people who access services, their families and carers and wider communities in the co-design and co-production of quality improvement and research projects.
Advanced level
- Role model meaningful allyship, supporting less experienced colleagues from marginalised and under-represented groups in their research-related development.
- Proactively collaborate with others to develop and deliver research and quality improvement projects, simultaneously learning from them and providing the opportunity for others to learn and develop at levels appropriate to them.
- Develop and nurture collaborative multi-disciplinary links between practice and research through networking with other practitioners, academics, university research departments / teams, clinical trials units, industry, practice-based and other researchers.
- Actively encourage and facilitate the equitable participation of people who access services, their families and their carers and wider communities in quality improvement and research initiatives, including through networks to help inform and design projects.
- Plan and ensure effective communication between partners, stakeholders and research teams, using communication approaches, tools and channels that meet the needs of particular audiences and individuals.
- Proactively participate in and grow research networks to engage with colleagues, support own career development, respond to opportunities, and facilitate the engagement of less experienced colleagues.
Consultant level
- Promote anti-racist and anti-discriminatory practices and allyship, the importance of diversity in all its forms, and equity in access to research-related opportunities and career progression.
- Sustain collaborative relationships with research teams working in related fields of practice to identify and address practice-based research priorities.
- Sustain collaborative, multi-disciplinary and multi-sector partnerships at organisational or national level or beyond, to generate and advance the implementation of new knowledge.
- Encourage, inspire and work with others to actively build research capacity and capability, including amongst public contributors, through collaborations and external relationships that reach beyond the organisation.
Research Capabilities Domain 6. Supporting research-related development in others
Recognising the collective effort required to build research capability and capacity, the Supporting research-related development in others identifies capabilities associated with practitioners at any level supporting those with less experience to develop their own research-related capabilities.
Entry level
- Role model the consistent use of evidence-based, person-centred best practice.
- Role model a proactive approach to addressing own identified learning and development needs, supporting and collaborating with others to do the same.
Enhanced level
- Support colleagues with less experience to access, understand, appraise and translate evidence into practice.
- Support the development of less experienced colleagues’ awareness and appreciation of the roles of audit, service evaluation, quality improvement and research activities in service delivery and development.
- Contribute to the support and supervision of pre-registration learners on practice placements, role modelling a commitment to evidence-based practice and linking them with local active trials / studies and the like.
- Explicitly draw on up-to-date research relevant to the discipline when contributing to education, training and professional development activities.
Advanced level
- Effectively use a range of approaches and techniques to support learning and development, showcasing up-to-date data and findings from research and service development projects.
- Foster the development of critical appraisal skills to facilitate understanding of what good research looks like and how to effectively and safely implement findings.
- Support, organise and promote professional development and educational events / activities to equitably build the capability of colleagues to engage in audit, service evaluation, quality improvement and research.
- Support awareness of the availability of local and national research-related resources and opportunities amongst those with less experience.
- Engage in peer support, mentorship and supervision of less experienced colleagues, including those undertaking academic qualifications, to support development and nurture talent.
- Provide learners and practitioners with opportunities to experience undertaking or contributing to research.
- Support learners and less experienced practitioners to publish, disseminate, promote and implement the outcomes / findings of their quality improvement and research projects.
Consultant level
- Facilitate collaborative links that support the effective and coherent integration of practice, research and education.
- Guide and enable the evidence-based learning of others through approaches that reflect contemporary issues and thinking, research evidence, and the opportunity to learn from errors.
- Educate and guide those with less experience, including public contributors, in the appropriate selection and use of research design, methods and techniques, data collection, management and analysis, and relevant supporting digital technologies.
- Educate specialist and non-specialist audiences about complex research-related ideas and theories.
- Supervise research projects undertaken by pre- or post-registration learners.
- Proactively and equitably support and facilitate the research-related career development of others.

Research Capabilities Domain 7. Leading and managing research projects and teams
Capabilities within the Leading and managing research projects and teams domain are those that provide the foundation for effectively stepping into research project leadership roles, managing associated staff and resources, and overseeing quality.
Entry level
- Actively contribute (at a level appropriate to own knowledge, skills and experience) to developing, embedding, expanding or sustaining a culture of research engagement within own service or department.
Enhanced level
- Act as a local champion to encourage and inspire colleagues to engage in, and with, inquiry and research.
- Demonstrate critical thinking to identify problems and research questions relevant to practice and policy.
- Prioritise the needs and priorities of the local population when planning quality improvement or research projects.
- Take the lead on small-scale service improvement projects.
- Apply for small-scale research-focused developmental opportunities and funding, with the support of, or in partnership with, more experienced colleagues.
Advanced level
- Promote a culture in which practice is continuously measured, evaluated, reviewed and improved through quality improvement and research initiatives.
- Support colleagues to obtain, collate, measure, analyse and evaluate data through audit, service evaluation and quality improvement projects and to translate their findings into practice.
- Act as a service level research champion, articulating the benefits of engaging in, and with, research, motivating, encouraging and inspiring others to do so.
- Generate and recognise viable ideas and opportunities for research and quality improvement projects and, acknowledging the contribution of others, work collaboratively with more experienced colleagues to shape research questions and contribute to funding applications.
- Recognise relevant organisational and national policy drivers and priorities when planning and reporting on quality improvement or research activities.
- Effectively consider the environmental impact of research and the methods by which it can be measured.
- Demonstrate understanding of ethics related to applied research, advising and guiding those with less experience accordingly.
- Contribute to the development of competitive grant funding applications.
- Demonstrate awareness of research team roles and responsibilities, contributing to the development of supporting infrastructure and effective lines of communication.
Consultant level
- Facilitate the accessing of relevant data from a range of systems to contribute to research and quality improvement, tracking and benchmarking progress, and fostering accountability.
- Formulate research questions that respond to current and future population and national trends and digital technology, and challenge the status quo.
- Cultivate the embedding of a commitment to consider environmental impact and wider issues of sustainability in all research and quality improvement activity.
- Contribute to or lead high-quality research projects at organisational or national level to address recognised practice-based research priorities.
- Contribute to large scale national or international audit, service evaluation, quality improvement or other inquiry.
- Maintain oversight of the research of those with less experience across organisational departments and services in own area of practice.
- Develop a national profile as an innovative critical thinker and role model, leading research and quality improvement that contributes to understanding, evidence-based change and development within the profession or service.
- Draw on experience and expertise to provide constructive expert reviews of publishable material.

Research Capabilities Domain 8. Strategic leadership in research and knowledge mobilisation
The focus of the Strategic leadership in research and knowledge mobilisation domain is on capabilities associated with awareness of, influencing and leading research and knowledge mobilisation within broader organisational, national or international contexts.
Enhanced level
- Demonstrate understanding of the strategic vision for research within own profession and work setting.
Advanced level
- Demonstrate knowledge of advances and knowledge-gaps in own and related areas of practice and research, and how they relate to organisational and national policies and priorities.
- Champion the role of applied health and care research to transform service design and delivery and the outcomes and experiences of individuals and communities.
- Demonstrate commitment to stakeholder involvement in the identification and selection of research priorities and throughout the research process.
- Contribute to the development, implementation or review of service or organisational strategic plans for research.
- Demonstrate appropriate application of regulatory and legal frameworks to applied research in practice settings.
- Demonstrate understanding of a variety of research-related funding sources and how to access them.
- Report to or hold membership of research-related committees or boards, internal or external to employing organisation.
Consultant level
- Demonstrate thorough understanding of the strategic direction of and developments in own and inter-related fields, using this knowledge to enrich research and practice.
- Contribute to or lead the embedding of an organisational culture that values and enables equitable engagement in, and with, research and quality improvement initiatives.
- Inspire curiosity and build enthusiasm across a range of stakeholders to engage positively with evidence-based practice, quality improvement, research activity and improvement science to optimise the quality of services and the experiences and outcomes of individuals and communities.
- Contribute to or lead practice-based research capability and capacity building and the development of related local career development structures.
- Contribute to or lead the development, implementation or review of research strategies at organisational level or beyond.
- Ensure strategic processes are in place and regularly reviewed to facilitate the equitable participation of people who access services, their families and carers, wider communities, staff and learners in research, and in the co-design and co-production of research and quality improvement initiatives.
- Actively contribute to the development, embedding and regular review of research governance policies and procedures, supporting adherence across the organisation.
- Be an active member of senior level research-related committees or boards, research organisations or working groups, internal or external to employing organisation.
Appendices
Appendix 1 – Strategic alignment with existing strategies and frameworks
The Multi-professional Practice-based Research Capabilities Framework is specifically aligned to and compatible with:
- the Chief Nursing Officer for England (2021) Strategic Plan for Research,
- the Chief Midwifery Officer for England (2023) Strategic Plan for Research,
- the Allied Health Professions Strategy for England 2022-2027: AHPs Deliver,
- the Health Education England (2022) Allied Health Professions’ Research and Innovation Strategy for England,
- the Department of Health and Social Care (2022) The Future of Research Delivery: 2022-2025 Implementation Plan,
- the Nursing and Midwifery Council Standards of Proficiency for Registered Nurses,
- the Nursing and Midwifery Council Standards of Proficiency for Midwives,
- the General Osteopathic Council Practice Standards,
- the General Pharmaceutical Council Standards for Pharmacy Professionals, and
- the Health and Care Professions Council Standards of Proficiency for in-scope disciplines,
- the NHS England (2023) NHS Equality, Diversity and Inclusion Improvement Plan,
- NHS England Delivering a Net Zero NHS – July 2022,
- the Health Education England (2020) Digital Competency Framework for UK Allied Health Professionals,
- the Health Education England (2021) Digital Capabilities for the Pharmacy Workforce,
- the Psychological Professions Digital Competence Framework,
- the All-Ireland Nursing and Midwifery Digital Health Capability Framework,
- the Nursing and Midwifery Council (2020) Principles of Preceptorship,
- the NHS England (2022) National Preceptorship Framework for Nursing,
- the NHS England (2023) National Preceptorship Framework for Midwifery,
- the Royal Pharmaceutical Society (2019) Foundation Pharmacist Framework,
- the National Allied Health Professionals Preceptorship and Foundation Support Programme,
- the Institute for Apprenticeships and Technology Enhanced Clinical Practitioner Apprenticeship Standard, V1.1, approved 27May2021,
- the Health Education England (2017) Multi-professional Framework for Advanced Practice in England,
- the Health Education England (2020) Multi-professional Consultant Level Practice Capability and Impact Framework and self-assessment tool,
- the Academy of Healthcare Sciences (2021) Good scientific Practice,
- the Academy for Healthcare Sciences (2015) Standards for Proficiency for Higher Specialist Scientists,
- the Council of Deans of Health (2023) Allied Health Professions Educator Career Framework,
- the research strategies published by individual professional bodies and associations,
- the multi- and uni-professional source material informing the development of the Framework, as outlined in Appendix 3, and
- the forthcoming NHS England growth-based career planning concept and resources.
Appendix 2 – Guidance relevant to support workers, technicians, assistants, associate practitioners[6] and pre-registration learners.
Research-related capabilities relevant to health and care support workers, technicians, assistants and associate practitioners and pre-registration learners can be located in guidance such as:
- the Health Education England (2021) Allied Health Professions’ Support Worker Competency, Education and Career Development Framework (see Domain 6, p.29),
- Health Education England’s (2021) Maternity Support Worker Level 3 Curriculum (see Domain 4, Competency 13, p.61),
- the Institute for Apprenticeships and Technical Education (2023) Assistant Practitioner (Health) Apprenticeship Standard (see Duty 3 and 10),
- the Institute for Apprenticeships and Technical Education (2022) Healthcare Science Assistant Apprenticeship Standard,
- The NMC (2018) Standards of Proficiency for Registered Nursing Associates,
- the General Pharmaceutical Council’s (2020) Requirements for the Education and Training of Pharmacy Support Staff, and pre-registration learning and development standards and curricula
Appendix 3 – Source material informing the Framework.
Alongside the reference points defining and describing the four levels of practice and the expectations associated with them, a range of uni-and multi-professional frameworks (and similar) contributed to / informed drafting and development of the Multi-professional Practice-based Research Capabilities Framework. They include:
Appendix 4 – Engagement contributors
Responses to engagement opportunities during the development of the Framework include those received from:
Name Role / Organisation
Jane Brown – Pharmacy Dean, Health Education England *
Camille Carroll – Professor of Clinical Neuroscience, Newcastle University
Chief Nursing Officer for England’s Strategic Plan for Research Advisory Group members –
Gemma Clunie – Senior Clinical Academic Speech and Language Therapist, Imperial College Healthcare NHS Trust
Joy Conway – Professor of Respiratory Physiotherapy; Subject Matter Expert in Research for Advanced Clinical Practice, Health Education England * / NHSE Workforce Training and Education Directorate
Joanne Cooper – Head of Nursing Research – Research Transformation, NHS England
Council of Deans of Health –
Rob Crouch – Honorary Professor of Emergency Medicine; Subject Matter Expert for Consultant Practice, Health Education England *
Angela Douglas – Deputy Chief Scientific Officer, NHS England
Owen Driskell – Deputy Training Programme Director Higher Specialist Scientist Training (HSST) Programme, National School of Healthcare Science
Ruth Endacott – Professor of Clinical Nursing; Director of Nursing and Midwifery, National Institute of Health and Care Research
Carol Fawkes – Institute of Osteopathy and the National Council for Osteopathic Research
Liz Fenton – Deputy Chief Nurse, Health Education England *
Andrew Finney – Senior Lecturer and Researcher, School of Nursing and Midwifery and School of Medicine, Keele University
Julia Gamston – Consultant Nurse in Urgent and Emergency Care, Imperial College Healthcare NHS Trust
Fiona Gibb – Director Professional Midwifery, Royal College of Midwives
Annette Hand – Clinical Academic Professor of Nursing, Newcastle upon Tyne Hospitals NHS Foundation Trust and Northumbria University
Helen Hurst – Professor of Nursing and Consultant Nurse, University of Salford and Northern Care Alliance NHS Foundation Trust
Imperial College Healthcare NHS Trust consultant nurses –
Helen Janiszewski – Clinical Lead for Nursing and Midwifery Research and Innovation, Nottingham University Hospitals NHS Trust
Amit Kulkarni – Head of Research and Outcomes, Royal College of Speech and Language Therapists
Tony Lavender – Emeritus Professor; member of the Practice Board, British Psychological Society
Judy Lawrence – Research Officer, British Dietetic Association
Alison Leary – Professor of Healthcare and Workforce Modelling, London South Bank University
Pip Logan – Professor of Rehabilitation Research, Nottingham City Care Partnership and University of Nottingham
Lynn MacDiarmid – Advanced Nurse Practitioner, Leicestershire Partnership NHS Trust
Laura McEwen-Smith – National Programme Lead Medical Associate Professions, NHS England
Fiona Maxton – Research Lead, Nursing Research Team, Chief Nursing Officer for England’s office, NHS England
Anne McLoughlin – Lead Clinical Nurse Specialist Breast Care, University College London Hospitals NHS Foundation Trust
Sarah O’Brien – Chief Nursing Officer, NHS Lancashire and South Cumbria Integrated Care Board
Office of the Chief Scientific Officer, NHS England –
Claire Pegg – Regional Chief Research Lead, National Institute for Health and Care Research
Alison Richardson – Professor of Cancer Nursing and End of Life Care; Head of Nursing Research – Academic Leadership and Strategy, NHS England
Hazel Roddam – Subject Matter Expert for Allied Health Research, Health Education England * / NHSE Workforce Training and Education Directorate
Denise Ross – Head of Health and Care Professions Academic Development, Leeds Teaching Hospitals NHS Trust
Jane Sandall – Professor of Social Science and Women’s Health; Head of Midwifery and Maternity Research, NHS England
Jacqui Scrace – Assistant Director of Nursing for Children and Young People, NHS England, South West Region
Rachel Taylor – Director of the Centre for Nursing, Midwifery and Allied Health Professional-led Research, University College London Hospitals NHS Foundation Trust
Peter Thompson – Director of NIHR Academy Programmes, National Institute for Health and Care Research
Lee Tomlinson – Head of Research, Kent Community Health NHS Trust
Helen Walthall – Director of Nursing and Midwifery Research and Innovation, Oxford University Hospitals NHS Foundation Trust
Gillian Ward – Head of Research and Innovation, Royal College of Occupational Therapists
Amanda Weaver – AHP Preceptorship Workforce Lead, Allied Health Professions Preceptorship and Foundation Support, NHS England
Adrian Whittington – National Clinical Lead for Psychological Professions, NHS England
Julia Williams – Professor of Paramedic Science, College of Paramedics
* Health Education England merged with NHS England in April 2023 and became the Workforce, Training and Education Directorate
Appendix 5 – Glossary
|
Audit
|
The NHS Health Research Authority [accessed 06.01.2023] defines clinical [practice] audit as ‘a quality improvement process that seeks to improve patient care and outcomes through systematic review of care against explicit criteria and the implementation of change.’
|
|
Clinical or Practitioner Academic
|
Clinical and practitioner academics work concurrently in practice (in health or social care) and academic environments. They provide practice and research leadership to underpin excellent evidence-based service provision, with a focus on improving effectiveness, quality and safety (AUKUH, 2016; Carrick-Sen et al, 2019; DoH, 2012). A range of training and developmental pathways exist (see, for example, NIHR), commencing at the level of internships and extending to Senior Investigator schemes and beyond.
|
|
Digital literacy
|
Health Education England [accessed 04.01.2023] define digital literacy as ‘those capabilities that fit someone for living, learning, working, participating and thriving in a digital society.’ |
|
Implementation science |
‘Implementation science is the study of ‘methods to promote the systematic uptake of research findings and other evidence-based practices into routine practice … to improve the quality and effectiveness of health services.’ (Eccles and Mittman, 2006). It considers how to design and evaluate activities to support the adoption of interventions, what might be influencing behaviour or preventing change, and how well-engaged audiences and communities might be (Knowledge mobilisation and implementation – ARC (nihr.ac.uk) [accessed 20.01.2023]). |
|
Knowledge creation
|
Knowledge creation is the process of making knowledge generated by individuals / groups available, amplifying it and connecting it to existing knowledge (Nonaka & von Krogh, 2009). It’s the continuous combination, transfer and conversion of different kinds of knowledge, including practice-based experience, expert opinion, audits and service evaluation outputs, quality improvement projects, research findings, systematic reviews and best practice guidelines.
|
|
Knowledge mobilisation (or translation) |
‘Knowledge mobilisation is about sharing knowledge between different communities to support change and create impact … Blending and acting on knowledge from different communities leads to new ideas, innovations, and new ways of working. Sharing knowledge alone is dissemination. Knowledge mobilisation generates impact.’ (Knowledge mobilisation and implementation – ARC (nihr.ac.uk) [accessed 20.01.2023]) |
|
Quality improvement
|
The Health Foundation (2021) identify that quality improvement is centred on ‘giving the people closest to issues affecting care quality the time, permission, skills and resources they need to solve them. It involves a systematic and coordinated approach to solving a problem using specific methods and tools with the aim of bringing about a measurable improvement.’
|
|
Research
|
The UK Policy Framework for Health and Social Care Research (2017) defines research as ‘…the attempt to derive generalisable or transferable new knowledge to answer or refine relevant questions with scientifically sound methods. This excludes audits of practice and service evaluations.’
|
|
Research delivery |
Research delivery encompasses the initiation, or setting up, of a funded and fully approved study, and undertaking the ‘active’ phase during which the study protocol is implemented, participants are recruited, and data is collected. (Clinical Research Network | NIHR [accessed 03/08/2023]; Bradford Institute for Health Research [accessed 18.01.2023]) |
|
Research impact |
The Research Excellence Framework 2021 [accessed 18.01.2023] defines research impact as: ‘an effect on, change or benefit to the economy, society, culture, public policy or services, health, the environment or quality of life, beyond academia.’ |
|
Service evaluation
|
The NHS Health Research Authority [accessed 04.07.2023] defines service evaluation as ‘a set of procedures used to judge a pilot’s [or service’s] merit by providing a systematic assessment of its aims, objectives, activities, outputs, outcomes, and costs.’ Robust evaluation identifies not only whether an intervention worked, but also why and how, allowing lessons to be learned and shared (The Health Foundation, 2015).
|
Footnotes
[1] Support workers, senior support workers, technicians, assistants, assistant practitioners and associate practitioners work with and alongside the health and care professionals and in those disciplinary areas, playing an important and growing role in delivering of safe and effective care for people accessing health and care services and wider communities.
[2] Fraser S. & Greenhalgh T. (2001) Coping with complexity: educating for capability. British Medical Journal 323, 799–803.
[3] McGee P, Inman C Eds (2019) Advanced practice in healthcare: dynamic developments in nursing and allied health professions. 4th ed. Chichester: John Wiley & Sons.
[4] Brunner et al (2018) An eHealth capabilities framework for graduates and health professionals: Mixed-methods study. Journal of Medical Internet Research 20(5), DOI: 10.2196/10229
[5] Leary (2022) The Principles of Enhanced Level Practice
[6] Support workers, senior support workers, technicians, assistants, assistant practitioners and associate practitioners work with and alongside the health and care professionals and in those disciplinary areas, playing an important and growing role in delivering of safe and effective care for people accessing health and care services and wider communities.