Submission Guidance for Existing Programmes – Version 2.2 October 2022
Contents
- Introduction
- Programme Accreditation for Existing Programmes
- Submission of Mapping Documents and Evidence
- Examples of Evidence Submitted for Programme Accreditation
- Downloads
Introduction
The Centre for Advancing Practice was established to oversee the workforce transformation of advanced level practice, by establishing and monitoring standards for education and training, accrediting advanced level programmes, supporting and recognising educational and training equivalence, and growing and embedding the advanced and consultant practice workforce.
The Centre delivers this through key functions:
- Programme accreditation
- Recognition of education and training equivalence
- NHS England credentials
- Workforce solutions
Advanced Clinical Practice
The Multi-professional framework for advanced clinical practice in England was published in 2017. The framework includes the national definition for advanced practice as below, and standards to underpin multi-professional advanced level practice.
“Advanced clinical practice is delivered by experienced, registered health and care practitioners. It is a level of practice characterised by a high degree of autonomy and complex decision making. This is underpinned by a master’s level award or equivalent that encompasses the four pillars of clinical practice, leadership and management, education, and research, with demonstration of core capabilities and area specific clinical competence.
Multi-professional framework for advanced clinical practice in England.
Advanced clinical practice embodies the ability to manage clinical care in partnership with individuals, families, and carers. It includes the analysis and synthesis of complex problems across a range of settings, enabling innovative solutions to enhance people’s experience and improve outcomes.”
As part of its remit, the Centre runs the Programme Accreditation process for Education Providers currently offering Advanced Practice masters level programmes that demonstrate they meet the capabilities across the 4-pillars of the Multi-professional framework for advanced clinical practice in England and the Standards for Education and Training (SET).
Programme Accreditation
Currently within the Centre, only existing Level 7 Higher Education validated Advanced Practice programmes that fully map to the Multi-professional framework for advanced clinical practice in England and the SET will be considered for accreditation.
Accredited programmes are listed by the Centre and learners who successfully complete an NHSE-accredited education programme are subsequently able to evidence that they have completed an accredited advanced practice programme.
Benefits of Programme Accreditation
Programmes accredited by the Centre will be subject to a rigorous quality assessment process based on the evidence submitted by the Education Provider, to ensure the teaching, learning, assessment and development initiatives meet the capabilities
described in the Multi-professional framework for advanced clinical practice and the Standards for Education and Training.
Centre accreditation signals to prospective learners, employers, patients and carers that the education and training programme is deemed to meet the standards required and promotes best practice underpinned by the values of the NHS Constitution. Thus, the
benefits of Centre accreditation include:
- the award of a recognised quality mark for the accredited advanced practice programme;
- entry on the Centre’s list of accredited programmes;
- review, feedback and advice from peers;
- permission to use the Accreditation Digital Badge on your website and promotional and programme materials; and:
- permission to use the strap-line ‘This programme is accredited by NHS England’s Centre for Advancing Practice’ on website and promotional and programme materials.
Purpose
This guidance document sets out the purpose, process and guidelines for Education Providers applying for accreditation of a Level 7 Advanced Clinical Practice programme to demonstrate that they meet both the Multi-professional framework for advanced clinical practice and the Standards for Education and Training.
If you would like to discuss any aspect of these guidelines, please contact us via: england.acpprogrammeaccreditation@nhs.net
Programme Accreditation for Existing Programmes
Overview
Accreditation is programme specific, not per Education Provider. Accredited programmes must meet the tandards for Education and Training and the capabilities for advanced clinical practice described in the 2017 Multi-professional framework for advanced clinical practice in England.
An existing programme is defined as an Advanced programme offered by an Education Provider where at least one cohort of learners is normally expected to have completed one full year of the programme before an application is made for accreditation.
Key Criteria
Each programme submitted for accreditation:
- must fully map to the Multi-professional framework Advanced Practice capabilities and the Standards for Education and Training. Programmes that only enable partial fulfillment cannot be considered for accreditation.
- must be delivered at level 7 (as per the Framework for Higher Education Qualifications, QAA) and result in a postgraduate qualification that fulfills the required standards as detailed above.
- is normally expected to result in the award of a Master’s degree (e.g. Master of Science (MSc)).
- must include workplace-based learning with a summative assessment that contributes to the final award which is appropriate and relevant to the learner’s needs.
The Application Process
Prior to booking
Education Providers should discuss their interest in submitting for programme accreditation with their Regional Faculty team. Given the demand for accreditation, the Centre will work with Regional Faculty teams to develop a schedule for accreditation submissions that will enable support and maintain standards. Prior to booking, and agreeing a submission date, the Centre will require the following information:
- Your Education Provider details, name of programme(s) and codes for submission
- Programme validation dates
- Name and contact details of the programme lead and Head of Department (or equivalents)
The Centre recognises that producing a high-quality submission takes a significant amount of resource and time, so prior to committing, please ensure that you are familiar with the requirements for submission and have the time required. Extensions for submission will only be granted under exceptional circumstances.
How many booking slots will you need?
Currently, programme accreditation is conferred for individual Level 7 Advanced Practice programmes. Education Providers must book a slot for each programme that leads to a separate award.
For example, you must book and submit individual applications for each:
- MSc Advanced Clinical Practice (Apprenticeship)
- MSc Advanced Clinical Practice
- MSc Advanced Clinical Practice (Critical Care)
- MSc Advanced Neonatal Clinical Practice
This requirement is necessary to ensure each programme has a clear and auditable set of documentation for quality assurance and quality monitoring purposes. If you have any doubt about whether your programme requires one programme slot or more in relation to multiple programmes and pathways, please contact the Programme Accreditation team who will be able to help.
Summary of the Programme Accreditation Process
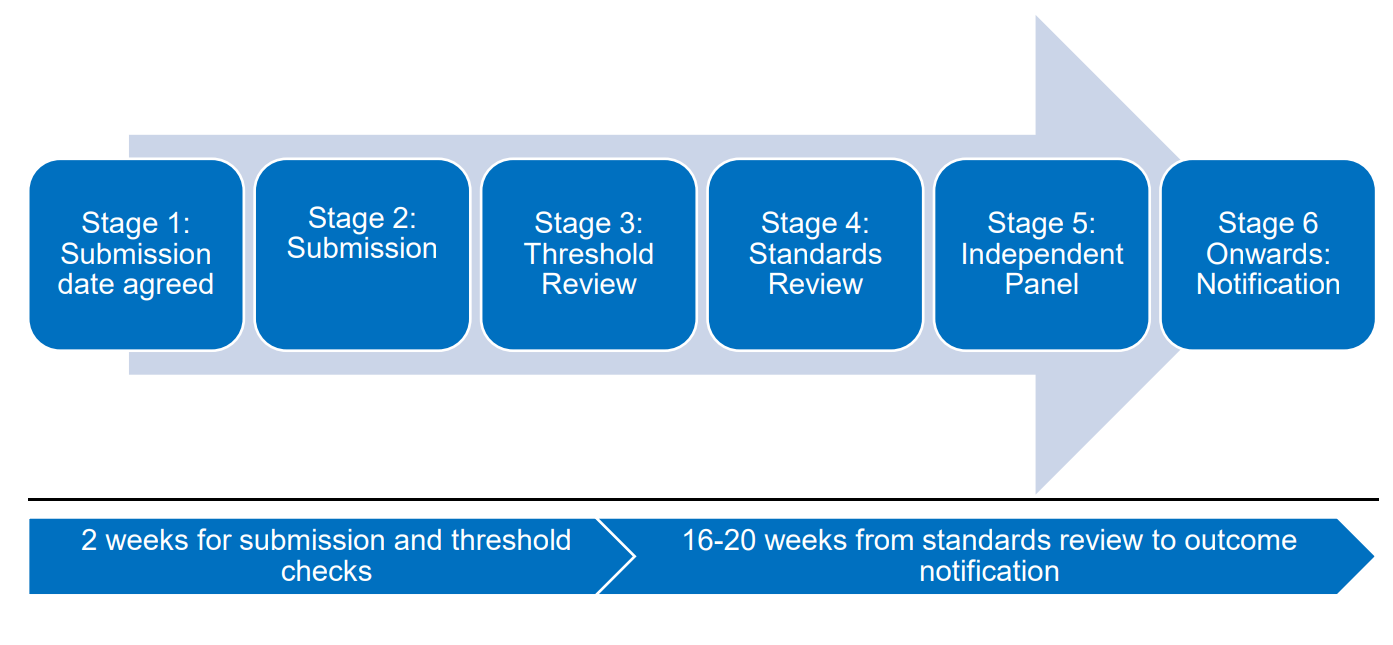
Stage 1: Submission date agreed
A submission date for programme(s) to start the accreditation process is agreed by all parties. Regional Faculty teams and the Centre will be available to support Education Providers with the submission process as required.
Once a submission date is agreed, the Centre will acknowledge the programme as “accreditation applied for”. This would be for your information only and for confirmation of a submission date and should not be shared/displayed as any form of endorsement or status of the programme.
Stage 2: Submission
Education Providers formally submit their programme (mapping documents and evidence) to the Centre SharePoint by the agreed date.
Please note, the SharePoint link(s) used to submit your programme(s) will be made available approximately one month ahead of the submission date.
Stage 3: Threshold Review
Following submission, a threshold review will be completed. This includes checking the integrity of the submission i.e., that mapping documents are fully completed, and all evidence links open. It also requires confirmation from the Regional Quality team that they are supportive of the programme to be accredited.
Once the Centre and Regional Faculty team are satisfied that the above has been met, the Programme Accreditation team can formally proceed with the next stages. The Programme Accreditation team will then notify the Education Provider that the threshold requirements have been met and that the submission has progressed to the review stages.
The threshold requirements can be found at the beginning of the Standards for Education and Training mapping document and are also set out below:
- The programme is an existing Advanced Practice programme.
- The programme is currently validated by a higher education institution (HEI) and full programme specification is submitted.
- The programme is at level 7 (in line with the Advanced Practice capabilities) and leads to a postgraduate award, normally a full MSc (Master of Science).
- There is a completed mapping document of the Advanced Practice Framework (capabilities) and the SET to specific programme components i.e. modules and assessments.
- If the programme includes any element that requires external validation/approval, such as independent prescribing, this must be evidenced. For example, you must include the current approval letter issued by the body providing the external validation/approval. For independent prescribing this is usually the General Pharmaceutical Council (GPhC) and/or Health and Care Professions Council (HCPC) and/or the Nursing and Midwifery Council (NMC).
- Local Office Advanced Practice Lead made aware of submission and indicates support for the programme.
- Regional Quality team made aware of submission and confirms if there are any educational quality issues with the programme, if an education improvement plan is in place or if they have any other concerns regarding the quality of the programme.
Stage 4: Standards Review
The submission will undergo a review by at least two reviewers who will independently assess the submission’s mapping documents and the supporting evidence. Following initial review, additional information can be requested to provide clarity or additional evidence. Should additional information be requested, advice on submitting this will be provided. Normally, the Centre offers two weeks for Education Providers to reply to such requests. Please note, any delay in responding to this additional information may lead to delays in the programme progressing through the accreditation process.
The purpose of the standards review is for each reviewer to undertake an independent review of the evidence submitted and form a judgement as to whether the programme has demonstrated that it meets both the Standards for Education and Training and the Multi-professional Advanced Practice capabilities.
Stage 5: Independent Panel
Once the review has been completed, a collective recommended outcome will be made by the reviewers. The Programme Accreditation team will submit this to an Independent Panel who will assess and review the recommendation.
The Panel’s role is to:
- consider and scrutinise the assessment of reviewers for the accreditation of programmes, moderating outcomes where required and ensuring that clear reasons are given for recommended outcomes;
- determine programme accreditation outcomes, ensure that the Centre’s standards and processes for programme accreditation are fairly, consistently and rigorously applied; and
- recommend programme accreditation outcomes to the Education Assurance Group at the Centre for ratification.
Stage 6: Notification
The decision made at the Independent Panel will normally be ratified with the Centre’s Education Assurance Group. At this point, the Education Provider and the Regional Faculty team will then be notified of the outcome. Outcomes from the submission would be:
- Accreditation without conditions
- Accreditation with conditions
- Accreditation not granted
Notification of the outcome will include written feedback confirming conditions (if applicable) and could include commendations and recommendations. The latter are suggestions that the Education Provider should consider to enhance the programme further. Where conditions have been specified, Education Providers will normally have 12 weeks to respond and will not be fully accredited until met.
Education Providers who have been fully accredited will then join the annual quality monitoring process and will also be sent the accreditation badge so that they can market their programme as accredited. Accredited programmes will also then be added to the
list of accredited programmes within the Centre.
Should a programme outcome be “Accreditation not granted”, the Centre will notify the Education Provider using the process described as above. The next steps for programmes with this outcome will be determined on a case-by-case basis, with involvement from all parties (Education Provider, Regional Faculty team and Centre).
Programmes that choose to re-submit after an accreditation not granted outcome are normally accredited from the point of the re-submission review. It is important to note that any re-submission is not backdated to the validation date as it would have been on
initial review.
The Centre’s Appeals and Complaints procedure can be accessed here.
Submission of Mapping Documents and Evidence
Mapping Documents
You must complete both the Multi-professional framework and Standards for Education and Training mapping documents in full for each submission
When submitting, please ensure you:
- use a file name for both documents that includes the date of the submitted document; the title of the programme; name of the Education Provider e.g. 20210922 MSc ACP HEE SET (name of education provider)
- use a file name for all other documents submitted in evidence that is consistent with the terminology used within the mapping documents
- quality check your submission – please ensure all hyperlink evidence fully opens independently
Signposting Evidence within the Narrative and Accompanying Documents
When mapping the programme to the capabilities and standards, consideration needs to be given to the narrative included within the mapping documents. Please ensure that the narrative supports the capability or standard and offers an explanation to how the programme and evidence submitted meets the requirements. Remember the reviewers will not be familiar with your programme and will be reviewing your submission based on the narrative and evidence submitted.
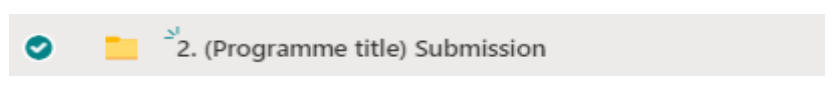
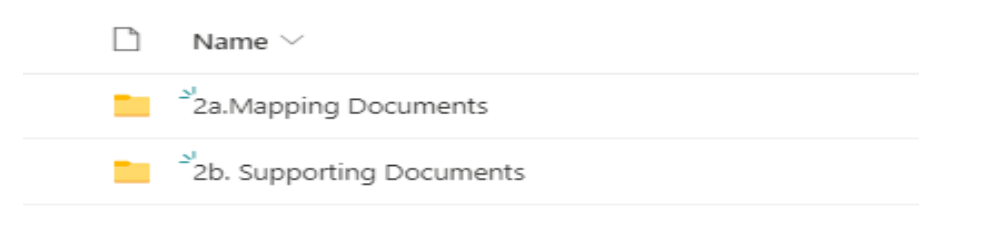
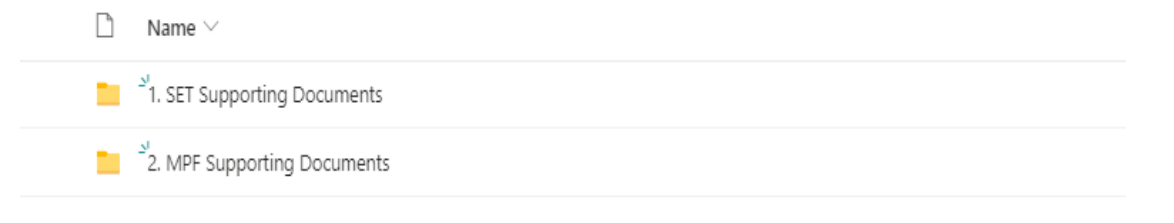
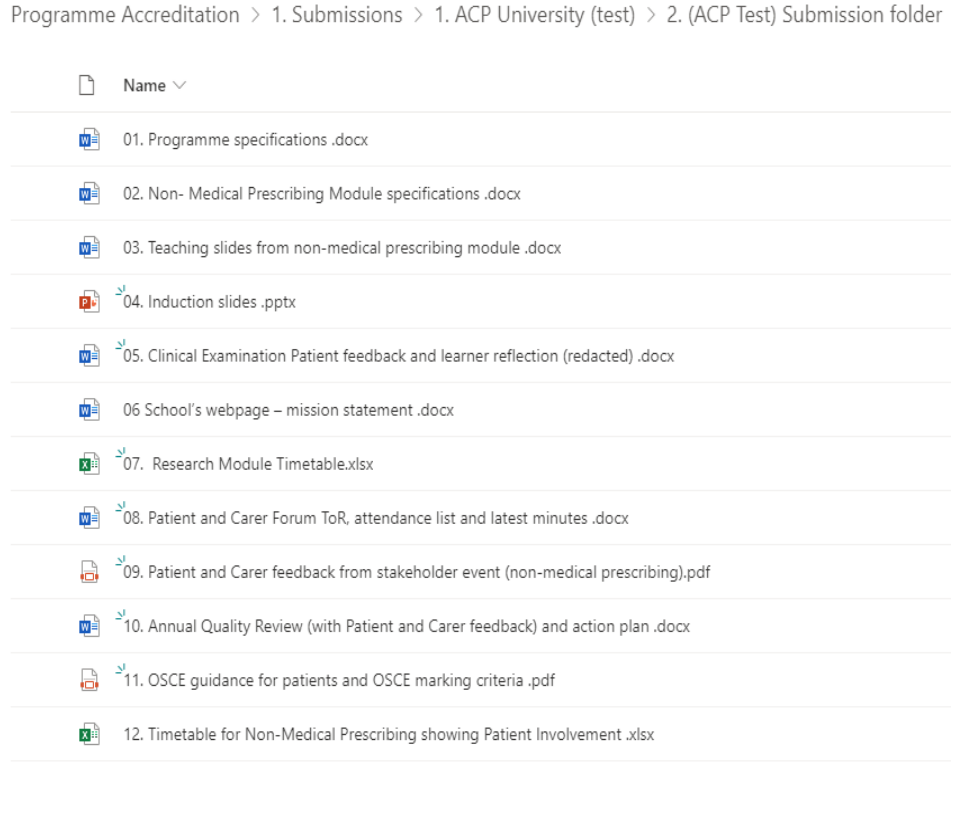
Advised Submission Structure
Following the review of submissions to date, please find below an advised structure for submitting your programme within the SharePoint folder. This submission structure will reduce duplication but ensures a structured and robust submission for review.
Please note for reviewers to successfully access the correct evidence, the document or evidence title within the mapping documents should be consistent and as it appears in SharePoint. Please also ensure that all documentation is titled with a numerical reference i.e. 01, 02, 03 etc.
Incomplete documentation will lead to delays in the programme’s accreditation process.
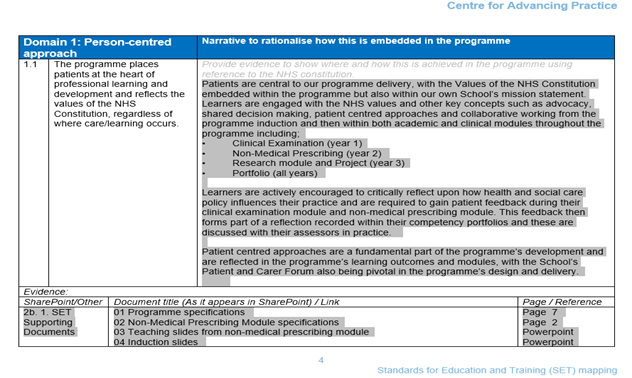
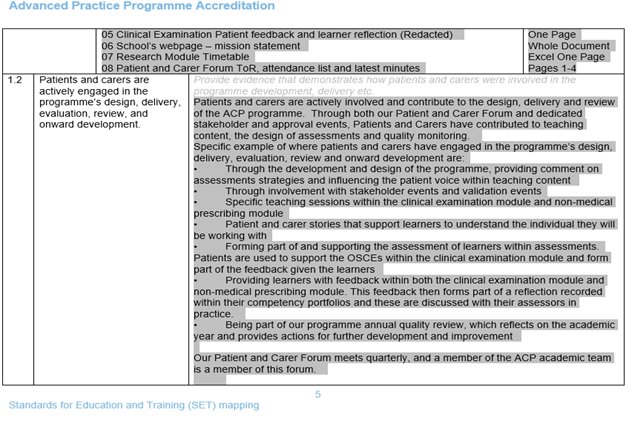
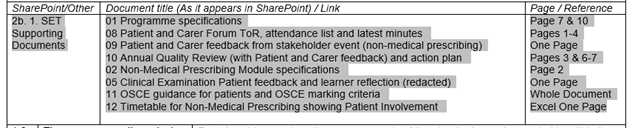
Below shows an example submission for SET 1.1 & 1.2. It provides a narrative and gives clear reference to the number and title of the evidence document along with the relevant page reference (s)
Supporting Evidence
It is important that you provide sufficient evidence to support your submission, and there will be many types of evidence that you could include. Examples include:
- programme and module specifications for both academic and clinical modules showing structure, delivery and content
- examples of assessments and marking schemes
- learner feedback and your response to that feedback
- module reviews and annual monitoring
- external examiner feedback
- minutes of meetings involving patients and carers, stakeholders and employers/supervisors
- clinical/work-based supervision, assessment, and support
- education provider staffing structures and up-to-date short CVs aligned to the requirements of SET
Of particular importance, you must include evidence of evaluation of your programme from your stakeholders. Some examples are given below.
Evidence should demonstrate:
achievement of the standards of the Multi-professional framework:
- Examples of learner engagement in reflection and peer review and evidence of impact including learner feedback
- Specific examples of inter-professional learning opportunities including learner feedback
a person-centred approach and the active engagement of patients and carers in the design, delivery, evaluation, review, and onward development:
- Examples of actions taken as a result of patient and carer feedback in the design of modules and review processes
- The Terms of Reference and Role Descriptors for patient representatives on formal programme oversight groups
- Feedback from patients and carer groups as part of the annual monitoring
- Evidence from patients and learners that “the learning process treats patients with respect, compassion and dignity”
a learner-centred approach and how learners receive regular feedback on their progress and are supported to embark on and progress through all stages of the programme:
- Examples of learner feedback and the actions taken in response to feedback and evidence of further evaluation undertaken to assess the impact of those actions
- Examples of feedback from clinical supervisors, assessors and mentors who provide support to learners and evidence of further evaluation undertaken to assess the impact of those actions
that the programme is demonstrably responsive to employers’ requirements and expectations in its design and delivery:
- Diagram showing how the programme team works in partnership with employers including employer involvement in programme governance
- Examples of employer feedback with actions plans and an evaluation of the impact of those action plans
that the team involved in the delivery of the programme has the requisite knowledge and skills to be able to contribute safely and effectively:
Include an up-to-date list of the core team for the programme summarising, for each team member:
- Role in the team
- Profession
- Regulator (if required for their role)
- Registration number (if required for their role)
- Qualifications (including teaching and learning qualifications)
- Expertise at advanced practice level relevant to their role in the programme
- Up-to-date short CVs or similar descriptor
Table 1. and Table 2. in section four below also provide additional advice on the types of evidence that has been provided in previous submissions to date. Please note, this is not exact or exhaustive but serves as a guide based on previous successful submissions.
Use of Optional Modules as Evidence
While optional modules form part of many programmes, they must not be used as the sole evidence of meeting a standard/capability. All capabilities within the Multi-professional framework need to be met by all learners completing the programme.
Information Sharing
By submitting your programme for accreditation with the Centre for Advancing Practice, the Education Provider agrees that your programme/organisation information may need to be shared with the following stakeholders:
- quality and regional faculty leads, for assurance purposes
- external reviewers, to understand the range of support and services provided, in order to meet student and patient needs.
- quality panels, for ratifying purposes
- information will be held securely on computers and an online SharePoint portal in accordance with the Data Protection Act 2018.
The purpose for processing this information is a core function of NHS England. For further information on NHS England’s privacy notice,
please click here.
Examples of Evidence Submitted for Programme Accreditation
Table 1. and Table 2. provide additional advice on the types of evidence that has been submitted in previous submissions to date. Please note, this is not exact or exhaustive but serves as a guide based on previous successful submissions.