Signpost for Continuing Professional Development (CPD): Published 2021
Introduction
In recent years the introduction of the advanced practitioner across the health care economy has provided an opportunity to develop the multi-professional workforce to meet the future healthcare needs of the population. The release of the NHS Long Term Plan1 has highlighted the importance for clearly articulating how targeted CPD for example can deliver an advanced practitioner multi-professional workforce that meets the mantra ‘right person, right place, right time’.
It is recognised that much has already been published on Continuing Professional Development (CPD) by professional2 and regulatory bodies34. The overall aim of CPD is to provide employees and employers with the ability to deliver high quality safe and effective person-centred patient care. It is also recognised that there are strong links between high quality CPD and improved patient safety5. However, the translation of these CPD requirements by individual stakeholders such as advanced practitioners and employers are complex, with many recommendations being so ‘high level’ they are open to individual interpretation as to the means of delivering and participating in quality CPD activities.
Aim
The overarching aim of this document is to enable discussion with advanced practitioners, professional and regulatory bodies with which to develop a clear signposting roadmap for CPD. For the purpose of the strategy the term advanced practitioner will denote both qualified and trainee advanced practitioners. This strategy has been written for use in England but should be transferable to the other devolved administrations.
Purpose
The purpose of this document is twofold, firstly to ensure alignment with current national standards, professional regulation requirements and academic best practice6. Secondly to signpost practitioners, Regional Faculty leads and employers to new and existing resources with which to undertake CPD and provide practitioners with an e-portfolio with which to record individual CPD activity once signed up to the Centre for Advancing Practice Portal.
It is not enough that advanced practitioners participate in CPD and revalidate in accordance with their professional bodies but that CPD is viewed as a platform to enable advanced practitioners to demonstrate the impact and value of their roles. This impact and value can be facilitated by developing an effective workplace culture and recognising the importance of the workplace as a place of learning7.
The NHS Long Term Plan outlines how healthcare delivery needs to change in order to provide high quality, person-focused care. The Plan also recognises that multi-disciplinary workforce models that include advanced practice are essential if this aspiration is to be recognised. The NHS Long Term Plan builds on the recommendations of the Next Steps on the NHS Five-Year Forward View8 and the Interim People Plan reinforcing the need for staff to have rewarding careers, have the right skills, experience and leadership to deliver safe and effective care.
Although there is a commitment to increase investment in CPD over the next five years9 how this is delivered against a background of current national recruitment and retention challenges is of utmost importance. Traditional methods of delivering CPD need to be augmented by incorporating advances in technology1011 which has been reinforced during the COVID 19 Pandemic. There are several Regional advanced practitioners’ networks within England which will need continuing support from NHS England Regional Faculties, employers and the consolidation of strong links with Higher Education institute (HEI). This is important as it will allow communities of practice to develop, creating opportunities for shared learning, research and supervision.
Multi-professional framework for advanced practice
There is a need to reshape the workforce to meet the future health needs of our population12. Whilst this not only provides opportunities for development of the multi-professional workforce it also raises the need for clearly defined levels of practice and education that meets the individual needs of this diverse workforce. In 2017 Health Education England (now NHS England) launched the Multi-professional framework for advanced practice13 defining advanced level practice as:skills, experience and leadership to deliver safe and effective care.
The framework describes capabilities which are mapped against level 7 (Master’s level) taxonomy and are built upon the four pillars of advanced practice14:
NHS England advanced practice also contains valuable resources on advance practice such as toolkits, programme accreditation and publications.
Advanced clinical practice is delivered by experienced, registered health and care practitioners. It is a level of practice characterised by a high degree of autonomy and complex decision making. This is underpinned by a master’s level award or equivalent that encompasses the four pillars of clinical practice, leadership and management, education and research, with demonstration of core capabilities and area specific clinical competence.
Advanced clinical practice embodies the ability to manage clinical care in partnership with individuals, families and carers. It includes the analysis and synthesis of complex problems across a range of settings, enabling innovative solutions to enhance people’s experience and improve outcomes.
Multi-professional framework for advanced practice in England
Continuing Professional Development
There are several definitions of CPD, that demonstrate the complexity of delivering effective CPD15.
systematic maintenance, improvement and continuous acquisition and/or reinforcement of the life-long knowledge, skills and competencies of health professionals. It is pivotal to meeting patient, health service delivery and individual professional learning needs. The term acknowledges not only the wide-ranging competences needed to practice high quality care delivery but also the multidisciplinary context of patient care
Executive Agency for Health Consumers (2013)16
In order to support workforces to continually develop and so provide high quality, safe and effective patient care, which also improves retention of experienced staff, CPD is crucial. The onus for maintaining CPD relies with the individual in order to maintain professional registration, however employers also have a responsibility to support individuals to maintain CPD. For the majority of advanced practitioners this may be evidenced within personal portfolio which may or not be linked to an e-Portfolio i.e. The Royal College of Emergency Medicine advanced clinical practitioners curriculum. However, there has been limited access to an e-portfolio with significant costs, so the majority of advanced practitioners have a traditional paper one.
There are a variety of recognised CPD activities such as:
- Attendance at organised learning events
- E-learning
- Evidence of audit/research/publications
- Simulation based education
- Reading and reflection on articles published in peer-reviewed biomedical journals
- Peer review activities
- Professional supervision
- Practice based small group learning
- Mandatory training
- HEI accredited modules
- Work based assessments such as case-based discussions
- Reflection
- Structed learning such as Intermediate Life Support, Advanced Life Support
Signpost for CPD
The overarching aim of this document is to provide advanced practitioners with the means with which to undertake person-centred CPD, which recognises the unique diversity of skills and expertise of the multi-professional workforce. It is also important that practitioners do not deconstruct the four pillars of advanced level practice but see them as an interlinked ‘map’ which allows them to work at an advanced level of practice. In order to ensure that the needs of the multi-professional advanced practitioner workforce are reflected in this signposting framework it has been co-produced, by developing a community of practice and through stakeholder engagements events. Thematic analysis of stakeholder feedback provided the following enablers and challenges for effective advanced practitioner CPD:
Enablers
- Dedicated and protected time in ‘job plans’
- Access to appropriate educational and clinical supervisors
- CPD development across all four pillars
- Signposting to relevant resources
- CPD hours and an electronic CPD ‘diary’
- Teleconferencing to allow attendance across the country
- E-portfolio that would link to accredited advanced clinical practitioner courses
- Adequate funding
- Technology
- Inhibitors
- Clinical pressure and management priorities
- Lack of funding and release from work to attend CPD activities
- Silo working with no national e-portfolio to upload evidence
- Language surrounding CPD activities (participatory/non-participatory)
- Ineffective job planning
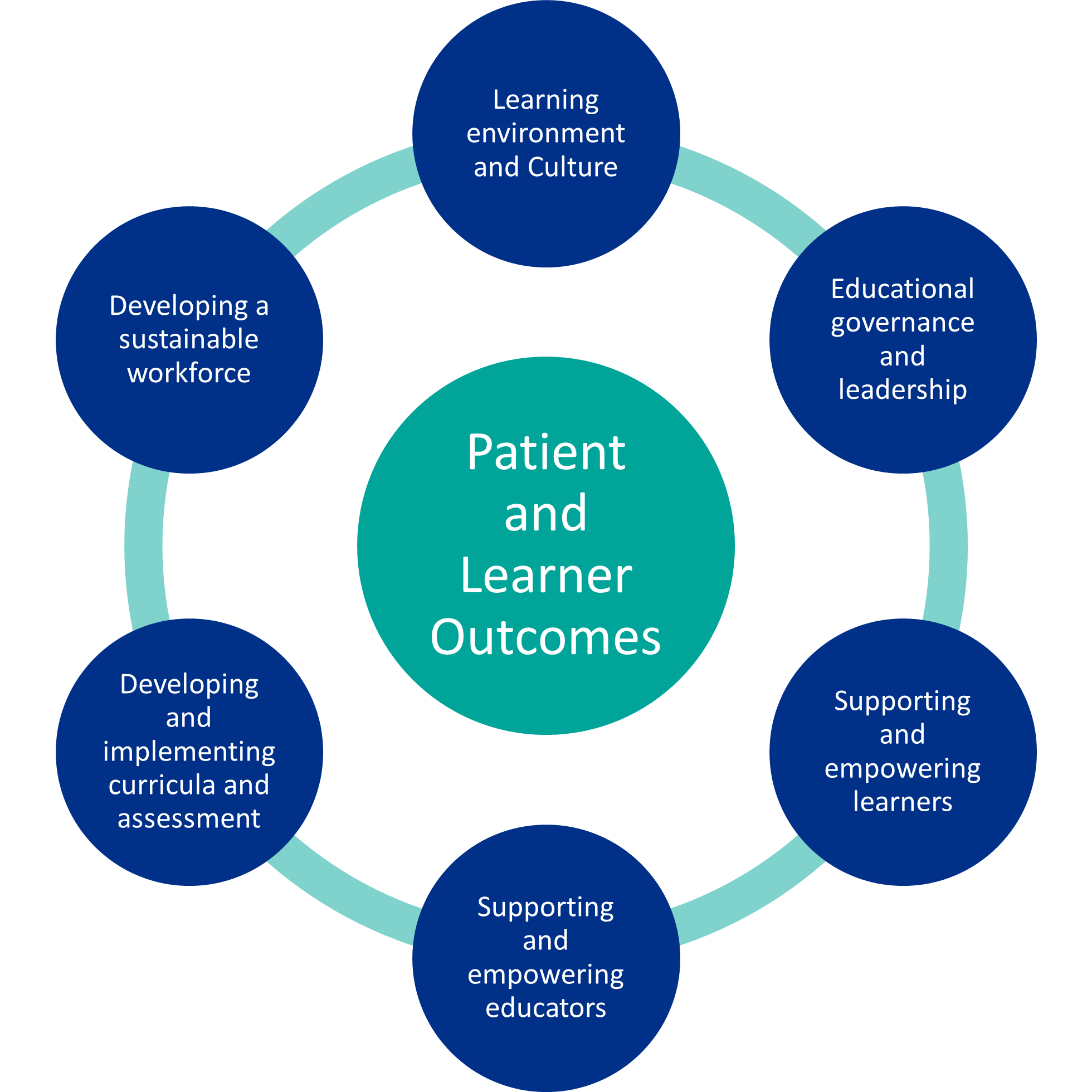
It is also important that the signposting recommendations are aligned with national quality standards and current research into CPD and person-centred care and reflects the NHS England Quality Framework 2019-202017 which is based on six domains (Fig.1.), with quality standards underpinning each domain.
There is a vast number of publications on CPD. However, a recent realist synthesis of effective CPD developed a theoretical framework for CPD built upon four theories:
- Transformation of Individual’s Professional Practice
- Transformation of Skills to Meet Society’s Changing Healthcare Needs
- Transformation of Knowledge to Enable Knowledge Translation
- Transformation of Workplace Culture to Implement Workplace and Organisational Values and Purpose
The four theories which contain context, mechanism and outcome (CMO) relationship, fit within the context of healthcare delivery with the arrows denoting the relationships which enable effective CPD (Fig.2.).

Whilst it is recognised that this is a conceptual framework the identified theories and CMOs can be applied to the role of the advanced practitioner such that CPD is seen as a crucial enabler with which to demonstrate value and impact of the role whilst adding to the wider evidence base of the advanced practitioner as part of the workforce. In summary:
- The workplace is recognised as a valuable place of learning
- Appraisals and workforce analysis should be used to identify learner’s development needs in order to plan and deliver a programme of development to meet the needs of future careers. One way in which this can be embedded within an organisational context is by dedicated advanced practitioner educator roles, who understand the role of the advanced practitioner and are able to act as a conduit between the workplace and organisation priorities. They are also able to act as a coordinator for educational supervisors for developing/trainee advanced practitioners
- By developing an understanding of change management and service improvement methodology, advanced practitioners are able to act as facilitators and change agents so providing an improvement focused positive work-based culture18
- Through effective self-development, clinical and compassionate leadership can not only promote organisational values but a positive patient experience by delivering patient-centred care that is both safe and effective
- Advanced practitioners are able to bring tacit knowledge and experience to deliver multi-professional team learning so helping professionals identify with the multiprofessional team
- Advanced practitioners should also use their CPD to develop their leadership skills to enable them to influence local and national strategic priorities
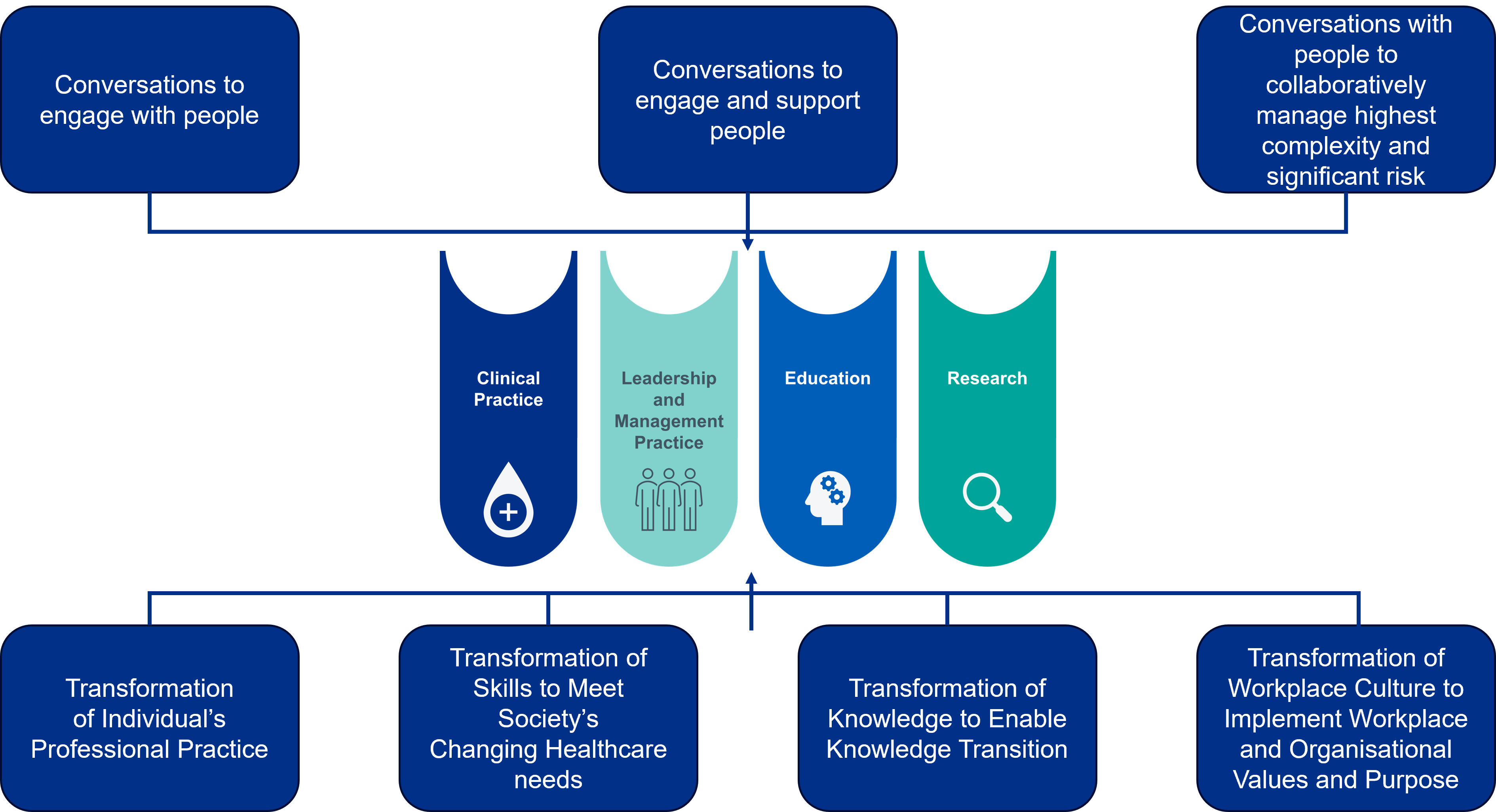
The Skills for Health Person-Centred Approaches19 is a framework which demonstrates how knowledge and activities overlap to influence a person-centred approach which put patients at the centre of health care delivery. The framework encompasses the values from the NHS Constitution20 and uses three steps to highlight inter-relationships between organisation and systems by using core values, relationship and communication skills (Fig.3.).

Much of the content resonates with the potential of the multi-professional advanced practitioners’ workforce to enable the aspirations of the NHS Long Term Plan and 5-year Forward View to meet the future needs of patients and their families. The framework also suggests tools with which to deliver workforce development and training (Appendix 1) advanced practitioners can ensure service delivery is person-centred as summarised below:
- Act as ‘whole system’ change agents as they are in the ideal position to use qualifying base profession, advanced practitioners’ skills/knowledge, tacit organisational knowledge and established networks to influence the system
- Advanced practitioners in primary care, frailty, First Contact Practitioners, respiratory, speech and language, pharmacy to name but a few have the opportunity to have conversations to enable and support people and manage complexity
- Reflection is an important aspect of developing personal CPD which allows for individuals to undertake transformative learning, problem solving, resilience and challenge behaviours21
- Advanced practitioners can deliver training and education to all members of the clinical workforce, for example utilising technology such as high-fidelity simulation to provide education and the ability for reflection, behaviour analysis, communication, decision making all of which are key aspects of a personcentred approach to service delivery
- Where their role requires it, advanced practitioners should utilise health coaching and motivational interviewing skills to enable patients to self-manage
Both the theoretical framework for CPD and the Skills for Health Person-Centred approaches framework are intertwined with the four pillars of advanced practice (Fig.4.). This is an important point to consider in developing advanced practitioner CPD as it could be argued that traditionally CPD was seen as a means of obtaining a specialist skill or means of updating one’s knowledge without necessarily identifying how this allowed for value and impact to be demonstrated.
In order to signpost CPD for advanced practitioners that incorporates the benefits of the aforementioned frameworks it is crucial that firstly advanced clinical practitioners see CPD as not something to be undertaken in isolation but something that is integral to everyday practice.
Secondly that CPD has to be incorporated into a well-balanced job plan which allows the individual to meet all four pillars of advanced practice. This can be conceptualised in the following four themes:
- Recording and evidencing CPD
- Accessing relevant training and development opportunities
- Accessing mentoring and supervision
- Leadership and educational development
Recording and evidencing CPD
Centre for Advancing Practice
The purpose of the Centre for Advancing Practice is to do the following:
- Enhance patient care and service delivery through strengthened transparency, governance and accountability arrangements for advanced clinical and consultant level practice
- Strengthen support for workforce development, mobility and progression that is responsive to changing population, patient, service delivery and workforce needs
- Achieve greater consistency in the education and professional development that supports advanced and Consultant-level practice
- Recognise advanced and consultant-level capabilities within the registered health and care professions, so that these can more strongly be drawn upon in models of care, service delivery and skill mix across multidisciplinary teams
The Centre for Advancing Practice will contain an e-portfolio functionality which members will also be able to use to record their CPD activity as required by the professional regulatory bodies.
The CPD section of the e-portfolio has been specifically designed to make it intuitive and easy to upload CPD activity. The design principles are:
- To continue to use the four pillars of advanced level practice as the framework against which all evidence is cross referenced
- Wherever possible adopt the same approach to CPD recording, that is being used by an applicant for the ‘Centre’ using the portfolio route and by those on a university course who are using the e-portfolio to gather evidence of their practice as an advanced clinical practitioner
- The e-portfolio will be built mobile first (designing a desktop site starting with a mobile version), which means that a CPD application will be available to allow members to quickly gather evidence of their CPD using mobiles/ tablets
It is envisaged that by making it intuitive to capture and upload CPD activity, it will encourage the advanced practitioner to utilise the e-portfolio as part of everyday practice rather than viewing it as a repository to be used when an individual is required to maintain professional membership. Whilst it is recognised undertaking CPD is the individual’s responsibility in order to meet the needs of their regulatory bodies, it is recommended that an adequate level of CPD to reflect their role as an advanced practitioner is undertaken.
In providing an e-portfolio it is envisaged that this will encourage members of the Centre for Advancing Practice to collect a suite of CPD activities which can then be used to inform appraisals, career development and revalidation requirements.
Accessing relevant training and development opportunities
e-learning for Healthcare
e-Learning for Healthcare (e-LfH) is a NHS England programme which was formed in 2007 and provides over 210 ‘blended learning’ e-learning programmes available to both the medical and multi-professional workforce.
With such a comprehensive suite of programmes, finding a selection that would suit the diverse needs of the multi-professional advanced practitioner workforce can be challenging. Therefore, as part of this strategy a collaborative piece of work was undertaken with e-LfH which enabled the programmes to be searched using the four pillars of advanced practice as keywords.
The programmes can be accessed by https://portal.elfh.org.uk and found using the search tool by typing the following acronyms in:
- ACPCP – Clinical
- ACPLM – Leadership and Management
- ACPE – Education
- ACPR – Research
Scholarships/fellowship opportunities
One way in which advanced practitioners can develop professionally and experience different ways of delivering advanced practice is by applying for fellowships or scholarships. The Florence Nightingale Foundation awards scholarship annually for nurses and midwives. The scholarships allow individuals to not only develop their careers but to also network, impact on policy/practice, personal development through adding to the existing evidence base.
The Health Foundation provide fellowships which directly relate to the four pillars of advanced practice. Fellowships include:
- Quality Improvement
- Leadership
- Improvement science
The National Institute for Health Research also have fellowships to develop research knowledge and careers such as Clinical academics. Fellowships and studentships are also available from the Medical Research Council and include:
- Doctoral training partnership
- Clinical Research Training Fellowship (CRTF)
- Senior Clinical Fellowship (SCF)
Another opportunity to undertake a fellowship is with the Winston Churchill Memorial Trust. The Churchill Fellowship started in 1965 and is
comprised of eight themes, one of which is ‘Health and Wellbeing’. The fellowship allows UK citizens to travel around the world to seek new experiences and solve problems.
Below are two exemplars from advanced practitioners who have recently undertook Churchill Fellowships:
Hannah Morley – Advanced Physiotherapist Practitioner, FCP, Winston Churchill Fellow Gloucestershire Health and Care NHS Foundation Trust
Kate Knowles – Operational Lead ACP for Medicine, Nottingham University Hospitals NHS Trust. Churchill Fellow 2017
It is evident that scholarships and fellowships afford advanced practitioners’ unique opportunities for professional CPD across the four pillars of advanced practice and as importantly to develop skills to demonstrate the impact and value advanced practitioners can bring to patient care and service delivery.
Accessing mentoring and supervision
An exemplar of how technology can be used to aid peer supervision for example in advance practice is Community Healthcare Outcomes Project (ECHO™).
Extension of Community Healthcare Outcomes Project (ECHO™)
Project ECHO was launched in 2003, following a healthcare initiative by a liver disease specialist who developed a free educational model which allowed him to expand the delivery of Hepatitis C care by mentoring community providers in New Mexico22 23.
Project ECHO is not ‘telemedicine” but rather ‘telementoring” where participants maintain responsibility for the care of patients but are able to receive specialist education and development regarding aspects of care. In the United Kingdom there are several sites using Project ECHO, one of these sites is St. Luke’s Hospice in Sheffield which is a ‘superhub’. They have facilitated for example communities of practice in dementia care, care homes and support for family carers
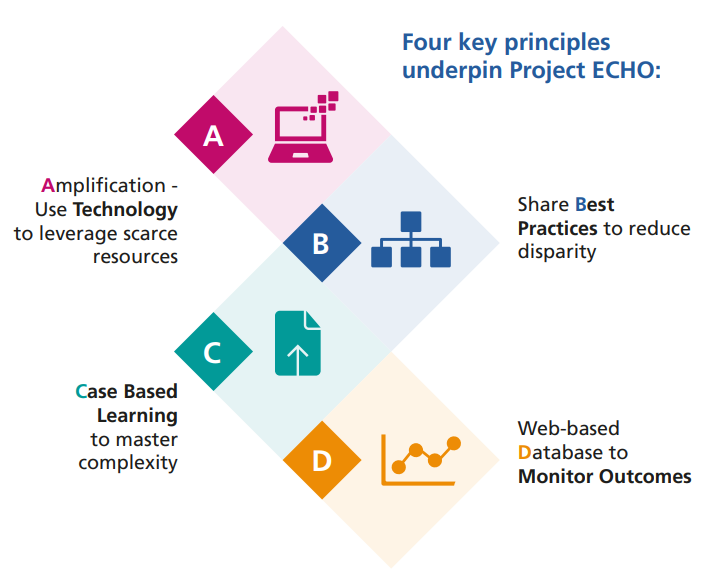
Across England there are already well-established networks of advanced practice, which if grown into Communities of Practice would provide a unique opportunity for advanced practitioners CPD. St. Luke’s Hospice in conjunction with South Yorkshire and Bassetlaw Faculty for Regional Advanced Clinical Practice undertook two pilots involving Project ECHO. The pilot’s involved First Contact Physiotherapist’s (FCP) and Primary and Community Care advanced practitioners regarding mental health, supervision and specialist education on subjects identified in knowledge events. Another benefit of using Project ECHO is that the pilots have enabled advanced practitioners from the across England to participate, so enabling targeted CPD and the sharing of different experiences. The pilots have been completed and the evaluation can be seen below:
The FCP/AP MH ECHO pilot was undertaken between April and September 2020 with a group of 11 FCP’s and 32 AP MH.
The ECHO session was evaluated as:
- ECHO sessions were easily accessible, non-judgemental interactive and well organised
- They recognised that as FCPs they had the potential to become isolated and enjoyed the peer-peer supervision element.
- They enjoyed that they were able to access the sessions without having to travel and acknowledged that this meant they have been able to access the training even during lockdown/social distancing
- Participants really appreciated the resources sent out after the session including case study feedback
- Participants felt that the facilitation of the sessions encouraged engagement in the learning and the conversational element around a topic led to learning from peers that might not happen with an in-service training presentation
- Participants agreed or strongly agreed that the cases provided learning that they can use in their practice
- 80% agreed or strongly agreed that they would change their practice due to something that they had learnt in the sessions
- Participants agreed or strongly agreed that they will change their practice due to something that they learnt during the ECHO session
- 94% of participants agreed or strongly agreed that the subjects of the presentations were relevant to their role
- 78% of participants felt that they learnt something new from attending the ECHO sessions
Evaluation data provided by Jane Manson, Leadership Fellow for Project ECHO, St. Luke’s Hospice, Sheffield
Supervision
Where advanced practitioner roles are well established, many are familiar with using workbased assessments (WBAs), such as case-based discussions and reflection, which have been used by health care professionals for many years as a means of demonstrating capability24. All of the WBA’s require clinical supervision of the advanced practitioner and whilst it is acknowledged that supervision is well established within modern healthcare25 26 27it is usually profession focused and may require some adaptation for a multiprofessional advanced clinical practitioner workforce. With appropriate training, advanced practitioners are in a strong position to be able to offer multi-professional supervision28.
The supervision requirements for the advanced practitioner are covered in detail in Workplace Supervision for Advance Clinical Practice: An Integrated multi-professional approach to practitioner development.
Another potential role of the Centre for Advancing Practice could be providing advanced practitioners with a directory of clinical supervisors with whom to contact for targeted clinical supervision. This can also be used by regional and advanced clinical practitioner networks and Integrated Care Systems to reinforce clinical supervisor networks.
Leadership and educational development
Leadership
No one pillar of advanced practice has greater importance than the other. Whilst it may appear that there is a greater emphasis on advanced practitioners developing their clinical pillar, development of leadership skills is an integral part of the advanced level practice, whether it is providing clinical leadership within the workplace or influencing strategic priorities across the healthcare system29. There is limited research surrounding leadership and advanced practice.
However, a recent study themed leadership into either ‘patient-focused’ or ‘organisation and system focused’ leadership30 both of which correlate with the aforementioned person-centred approach and the realist synthesis which underpin this signposting framework.
There are a variety of funded programmes to enable advanced practitioners to develop their leadership skills. The Leadership and Lifelong Learning (NHS Leadership Academy) has a range of tools, resources, programmes and case studies with which to promote effective leadership with the NHS. A recent review of how the NHS Leadership Academy can support advanced practice identified the following key aspects which can further developed:
- Rosalind Franklin Programme meets the requirement for the multi-professional framework advanced practice in England (2017) leadership and management pillars. There is also a potential for the Centre for Advancing Practice to ‘credential’ the programme
- The Leadership and Lifelong Learning team works with the Centre for Advancing Practice to jointly develop a national approach to the accreditation of leadership programmes, modules and continuing professional development activities
- Regional teams to work with colleagues who are leading CPD for advanced practitioners to provide focussed practitioner support. This could be through a community of practice, access to career coaches, interactive webinars, leadership-focused masterclasses, mentoring
and action learning set facilitation
Regionally there are local academies such as the KSS Leadership Academy which offer a variety of resources ranging from system leadership to coaching. Another valuable resource that allows for individual leadership development is the Healthcare Leadership Model. The NHS Leadership Academy is also developing the NHS Leadership Model App which is currently in beta testing and can be used
via a desktop or mobile device. It is designed to capture, personal reflection on your leadership style and set goals and comment on leadership behaviours.
Innovative advanced clinical practitioner roles and targeted CPD
As advanced level practice develops there is a need to ensure that the diverse nature of the multiprofessional workforce CPD requirements are met will require collaboration between educators and employers31 if the potential that advanced practitioners bring to healthcare delivery is to be realised.
One such way is by developing academic roles for advanced practitioners. One way in which this could be achieved is by the development of joint appointments of advanced practitioners between NHS organisations and Higher Education Institute (HEI) following the Follett principles. Appointments such as this would not only provide a novel career pathway for advanced practitioners but could also
support the development of a clinical academic pathway as research is seen as a critical component of future of person-centred healthcare provision32 33.
Further information on clinical academic careers can be found at the Association of UK University Hospitals (AUKUH).
Another innovative approach to providing advanced practitioner CPD is the role of the advanced practitioner educator who ensure CPD is delivered within the workplace, incorporating adult learning principles, active learning, complex communication and decision making so creating effective learning experiences34. Examples of the benefits of these roles are:
Jennifer Riley – Interim Corporate Lead for Advanced Practice.
Trust Lead Non- Medical Prescribing.
ACP- Acute Medicine.
University Hospitals of Derby and Burton NHS Foundation Trust
James Pratt – Trust Lead Advanced Clinical Practitioner, Nursing and Midwifery institute. Nottingham University Hospitals
An example of a job description can be found in Appendix 2 with further details of how Nottingham University Hospitals have ensured CPD is intertwined within all aspects of day-to-day practice (Appendix 3).
The future of CPD delivery
COVID-19 has impacted on traditional approaches to and delivery of CPD, such as conference attendance, and face-to-face delivery of HEI modules. Therefore, it is reasonable to anticipate that there will be a shift to the greater use of technology to facilitate synchronous and asynchronous learning.
- Synchronous learning refers to a learning event in which learners are engaged at the same time. The benefits are immediate feedback and interaction. However, it is dependent on a fixed schedule, with some learners feeling they do not receive individual attention and is dependent on the skills of the instructor
- Asynchronous learning is a more learnercentred approach which although lacking real time interaction, offers a flexible, cost effective means of accessing learning. A potential limitation that learners can feel isolated, and they need to be self-disciplined
Technology, provides a huge opportunity for the advanced clinical practitioner workforce to not only participate in synchronous/asynchronous CPD that may not have been accessible or practical such as attendance at international conferences but also to utilise new educational resources for advanced practitioners to provide CPD. An example is the production of Podcasts such as The Resus Room or ED Educate.
There is a plethora of learning resources, which are outside the scope of this document to individually list. Examples of these resources:
- e-LfH
- NHS Library Services
- BMJ Best Practice
- Public Health England
- The Technology Enhanced Learning (TEL) Programme provides a framework for Simulation based education and has recently launched the Learning Hub (https://learninghub. nhs.uk) which not only provides access to e-LfH modules but also allows organisations to share resources. Again, this provides ACP’s with the opportunities to share learning and participate in CPD
- MindED is a free educational resource on mental health for children and Young people
- Centre for Pharmacy Postgraduate Educationoffer free learning for pharmacists and independent non-medical prescribers
- Script offers e-learning resources for prescribers
- Future Learn offers a variety of e-learning which can be accessed for free or with an annual subscription
- Oxford Medical Education (OME) provides free medical education resources
- CORE open access research papers
- RCNI Learning offers RCN members access to educational material
With COVID 19 the use of technology has evolved and has enabled students to access clinical placements and provides a platform with which to provide clinical supervision.
Another key enabler is the development of communities of practice within advanced practice. Communities of practice enable collective learning and support by groups of individuals with a shared expertise or interest. By embracing technology such as Project ECHO to deliver digital CPD and leadership it will allow existing advance practice networks to come together. This will enable the new regional advance practice faculty leads and the Centre for Advancing Practice to work collegiately to share best practice and develop a network of shared learning and supervision. The benefits of this would be to provide a consistent platform with which to develop advance practice but also by engaging advance practitioners to create regional faculties of learning so ensuring that the needs of all of the advance practice multi-professional workforce are met.
One thing is certain and that is the delivery of CPD is ever evolving which will require a ‘CPD imagination’ which is a new way of thinking of practising CPD differently to ensure effective healthcare delivery35.
Summary
This is one of several papers that will see the ‘Centre for Advancing Practice’ become the platform that will enable advanced practitioners to share best practice, education, research and begin the process of providing standardisation of advanced level practice within England.
It is recognised that this document cannot provide an in-depth evidence-based review of CPD but by acknowledging the evidence base has aimed to act as a ‘signpost’ with which to raise awareness, thus empowering individuals to develop focussed, relevant and collaborative approaches to CPD. The aspiration being that education moves away from traditional thinking of CPD attainment and place
CPD in the centre of everyday practice by embracing technology, opportunities, resources and new initiatives.
References
- NHS England. (2014). Five Year Forward View. https://www.england.nhs.uk/wp-content/uploads/2014/10/5yfv-web.pdf ↩︎
- Broughton W., and Harris G. (2018). Principles for Continuing Professional Development and Lifelong Learning in Health and Social
Care. Bridgwater. College of Paramedics. Available at: https://www.bda.uk.com/uploads/assets/3830abb3-e267-4f5c-a93e7c3aca843ffe/
cpdjointstatement.pdf ↩︎ - Nursing & Midwifery Council. (2019). Revalidation. Available at: https://www.nmc.org.uk/globalassets/sitedocuments/revalidation/howto-revalidate-booklet.pdf ↩︎
- Health & Care Professionals Council. (2019). CPD Standards. Available at: https://www.hcpc-uk.org/cpd/your-cpd/our-standards-for-cpd ↩︎
- NHS England. (2013). How to ensure that the right people, with the right skills, are in the right place at the right time. Available at: https://www.england.nhs.uk/wp-content/uploads/2013/11/nqb-how-to-guid.pdf ↩︎
- Maclaine, K. (2017). Principles document. Association of Advanced Practice Educators UK. Available at: http://aape.org.uk/wp-content/uploads/2015/02/AAPE-UK-Principles-Finalversion-22-9-17.pdf ↩︎
- Manley, K. Martin, A, Jackson, C. et al. (2018). A realist synthesis of effective continuing professional development (CPD):n A case
study of healthcare practitioners CPD. Nurse Education Today. 69. 134-141. Available at: https://www.sciencedirect.com/science/article/pii/
S0260691718302995 ↩︎ - NHS England (2019). NHS Long Term Plan. https://www.england.nhs.uk/long-term-plan/ ↩︎
- NHS. (2019). Interim People Plan. Available at:https://www.longtermplan.nhs.uk/wp-content/uploads/2019/05/Interim-NHS-People-Plan_
June2019.pdf ↩︎ - Topol, E. (2019). The Topol review: Preparing the healthcare workforce to deliver the digital future. Available at: https://topol.hee.nhs.uk ↩︎
- Watcher, RM. (2016). Making IT work: Harnessing the Power of Health Information Technology to Improve Care in England.
Available at: https://assets.publishing.service. gov.uk/government/uploads/system/uploads/attachment_data/file/550899/Watcher_Exec_
Summary_Accessible.pdf ↩︎ - Nuffield Trust. (2016). Reshaping the workforce to deliver the care patients need. Available at: https://www.nuffieldtrust.org.uk/files/2017-01/reshaping-the-workforce-webfinal.pd ↩︎
- NHS (2017). Multi-professional framework for
advanced clinical practice. Available at: https://advanced-practice.hee.nhs.uk/multi-professional-framework-for-advanced-practice/ ↩︎ - Manley, K. (1997). A conceptual framework for advanced practice: an action research project operationalising an advanced practitioner/nurse consultant role. Journal of Clinical Nursing, 6(3), pp179-190. ↩︎
- Manley, K. Martin, A. Jackson, C. et al. (2018). A realist synthesis of effective continuing professional development (CPD): A case study of
healthcare practitioners CPD. Nurse Education Today. 69.p134-141. [Accessed 1st June 2020]. ↩︎ - Executive Agency for Health Consumers. (2013). Study concerning the review and mapping of continuous professional development and lifelong learning for health professionals in the European Union. European Union. http:// ec.europa.eu/health//sites/health/files/workforce/ docs/cpd_mapping_report_en.pdf, ↩︎
- HEE. (2016) HEE Quality Strategy 2016-2020. Available at: http://www.oxforddeanery.nhs.uk/ pdf/HEE_Quality_Strategy_2016_2020.pdf ↩︎
- Manley, K., Sanders, K., Cardiff, S., Webster, J., 2011. Effective workplace culture: the attributes, enabling factors and consequences of a new concept. Int. Pract. Dev. J. 1 (2). ↩︎
- Skills for Health. (2017). Person-Centred Approaches: Empowering people in their lives and communities to enable an upgrade in prevention, wellbeing, health, care and support. Available at: https://www.skillsforhealth.org. uk/news/latest-news/item/576-new-frameworkto-promote-person-centred-approaches-inhealthcare ↩︎
- NHS. (2015). The NHS Constitution: The NHS belongs to us. Available at: https://assets. publishing.service.gov.uk/government/uploads/ system/uploads/attachment_data/file/480482/ NHS_Constitution_WEB.pdf ↩︎
- Howell, R. (2017). Reflection and CPD- what’s it all about? Available at: https://www.rcog.org.uk/ globalassets/documents/members/membershipnews/og-magazine/summer-2017/cpd-andreflection.pdf ↩︎
- FICM. (2015). Advanced Critical Care Practitioners – CPD & Appraisal Pathway. Available at: https://www.ficm.ac.uk/sites/ default/files/accp_cpd_appraisal_pathway_-_ version_2.2_-_march_2020.docx.pdf ↩︎
- Arora, S. Thorton, K. Mutana,G.(2011). Outcomes of Treatment for Hepatitis C Virus Infection by Primary Care Providers. The New England Journal of Medicine. 364:2199-207. Available at: https://www.nejm.org/doi/ pdf/10.1056/NEJMoa1009370 ↩︎
- General Medical Council. (2017). Open Designing and maintaining postgraduate assessment programme. Available at: https:// www.gmc-uk.org/education/standardsguidance-and-curricula/guidance/designingand-maintaining-postgraduate-assessmentprogrammes ↩︎
- Harding, D. (2019). Practitioner permeability and the resolution of practice uncertainties: a grounded theoretical perspective of supervision for allied-health professionals (PhD thesis0, St. George’s, University of London. Available at: https://eprints.kingston.ac.uk/43854/6/ Harding-D-43854.pdf ↩︎
- COPMeD. (2020) A Reference Guide for Postgraduate Speciality Training in the UK. The Gold Guide 8th Edn. Available at: https://www. copmed.org.uk/gold-guide-8th-edition/ ↩︎
- Academy of Medical Royal Colleges. (2020). Developing Professional Identity in multiprofessional teams. Available at: https://www. aomrc.org.uk/reports-guidance/developingprofessional-identity-in-multi-professionalteams/ ↩︎
- NHS Future Forum (2012) Education and training: next stage – a report from the NHS Future Forum. Available at: http://www.dh.gov. uk/prod_consum_dh/groups/dh_digitalassets/ documents/digitalasset/dh_1 32025.pdf ↩︎
- Department of Health (2012) Liberating the NHS: Developing the Healthcare Workforce from design to delivery. Available at: http:// www.dh.gov.uk/prod_consum_dh/groups/dh_ digitalassets/documents/digitalasset/dh_1 32087. pdf ↩︎
- Lamb, A. Martin-Misner, R. Bryant-Lukosius, D. et al. (2018). Describing the leadership capabilities of advanced practice nurses using a qualitative descriptive study. Nursing Open. Available at: https://onlinelibrary.wiley.com/doi/ epdf/10.1002/nop2.150 ↩︎
- Council of Deans. (2018). Advanced clinical practice education in England. Available at: https://councilofdeans.org.uk/wp-content/ uploads/2018/11/081118-FINAL-ACP-REPORT.pdf ↩︎
- Ramani, S. McMahan,G.T. Armstrong, E.G. (2019). Continuing professional development to foster behaviour change: From principles to practice in health professions education. Medical Teacher. 41 (9). Available at: https://doi. org/10.1080/0142159X.2019.1615608 ↩︎
- Yamagata-Lynch, L.C. (2014). Blending Online Asynchronous and synchronous Learning. International Review of Research in Open Distributed Learning. 15 (2). P 189-192. Available at: https://www.erudit.org/en/journals/ irrodl/2014-v15-n2-irrodl04928/1065292ar/ ↩︎
- Cumming, G. McLennan, M. (2005). Advanced Practice Nursing – Leadership to Effect Policy Change. Journal of Nursing administration. 35 (2). p 61-66. [Accessed 20th June 2020]. ↩︎
- Kitto, S. (2019). Opening up the CPD Imagination. Journal of Continuing Education in Health Professions. 39 (3). P 159-160. Available at: https://journals.lww.com/jcehp/Citation/2019/03930/Opening_up_the_CPD_Imagination.1.aspx ↩︎
Appendix 1
Appendix 2
Appendix 3
Acknowledgements
This signposting document was developed from April 2019 to March 2021. There have been numerous contributions through email, telephone correspondence and stakeholder events. A community of practice comprising of multi-professional advanced practitioners from all provider settings, academics and service leads was also developed which allowed for an inquiry-based approach.
The work was authored by Ian Setchfield, Acute Care Consultant Nurse, East Kent Hospitals University Foundation NHS Trust