Advanced practice workplace supervision – Minimum standards for supervision (2020)
Introduction
High quality supervision for healthcare professionals moving into trainee advanced practice roles is essential for supporting the development of confidence and capability and underpins patient and practitioner safety. NHS England Workplace supervision for advanced clinical practice provides further in-depth, evidence based information and recommendations on how to develop quality supervision in the workplace. The following guidance is for supervisors, managers, employers, and trainee advanced practitioners to advise of the Centre for Advancing Practice minimum expected standards for supervision.
Why do we need supervision?
The transition from experienced professional to trainee advanced practitioner and then to qualified advanced practitioner requires significant adjustment. Periods of feeling disconnected, lack of familiarity with the new situation and arrival of a new set of unfamiliar expectations are characterisation of transition. Work role transition requires a change in identity and the development of new knowledge and skills, as well as a change in behaviour. High quality supervision can support this transition.
Non-urgent advice: Minimum standards:
To ensure high quality supervision for trainees:
- Supervision for the trainee advanced practitioner is mandatory.
- The trainee must have a named, allocated co-ordinating education supervisor before commencing training in advanced practice.
- Throughout the period of training, there must be a minimum of one hour of scheduled supervision every week; of which one in four (once a month) is a scheduled hour with the co-ordinating education supervisor (see page 3 for definition of role).
- In certain practice contexts, where there is high risk, it will be necessary to debrief/provide daily supervision to ensure patient and practitioner safety.
Where a health professional is developing in advanced practice in a specialty/role with a nationally agreed curriculum, supervision arrangements should be guided by the relevant specialty curriculum.
Where no national curriculum exists, agreement of capabilities to be achieved at advanced level must be approved by the employer.
Who can supervise?
Supervisors:
- Come from the multi-professional workforce and do not need to hold the same professional registration as the trainee.
- Have expert knowledge of the area of practice they are supervising.
- Have experience as an educator and are a skilled facilitator able to support learning, development, assessment and verification of competence and capability.
A trainee advanced practitioner may need more than one supervisor to meet their needs across the 4 pillars of advancing practice:
- A co-ordinating education supervisor who provides a consistent relationship throughout training and must have an in-depth understanding of the advanced practitioner’s role within the speciality.
- Associate workplace supervisors who work collaboratively with the co-ordinating education supervisor to guide trainee development in one or more of the 4 pillars of advancing practice.
Non-urgent advice: Minimum standards:
The co-ordinating education supervisor must:
- be an experienced practitioner.
- have completed some formal supervisor development. Examples of formal training include: Clinical educator programmes; PgCert in clinical education; practice educator programmes; local supervisor training courses.
- have completed the “Supervisor readiness checklist’ (Appendix 2.0) before agreeing to take on the role.
If the co-ordinating education supervisor is an advanced practitioner:
- must have been working at advanced level for a minimum of 3 years. There should be clear justification for an advanced practitioner with less than 3 years’ experience undertaking this role.
Associate workplace supervisors must:
- demonstrate expert knowledge and capability of the area of practice they are supervising.
There must be a delegate or replacement supervisor in the event the co-ordinating education supervisor is on leave for a prolonged period of 4 weeks or more.
Where supervisor standards exist in a specific area of advanced level practice (e.g. as set by a capability or curriculum framework, including a credential specification), these generic standards should be used to complement (rather than override) them.
Detailed definitions of these roles are available Health Education England’s (2020) Workplace Supervision for Advanced Clinical Practice.
When should supervision take place?
The amount of supervision needed by a trainee advanced practitioner will vary dependent on the stage they are at, their personal learning needs and the practice context.
Non-urgent advice: Minimum standards:
- To have a first meeting with the identified co-ordinating education supervisor at induction or no later than four weeks before commencing training to discuss a supervision plan.
- Throughout the period of training, a minimum of an hour of scheduled supervision every week; of which one in four (once a month) is a scheduled hour with the co-ordinating education supervisor.
- Time should be allocated in the job plan for both supervisor and trainee.
- Remaining weekly supervision may be with the co-ordinating education supervisor
OR with an identified associate supervisor with knowledge and skills matched to the curriculum/competence/ capability focus of supervision for that week.
Scheduled supervision in advanced clinical practitioner apprenticeships should be within the off-the-job training time
What does good supervision look like?
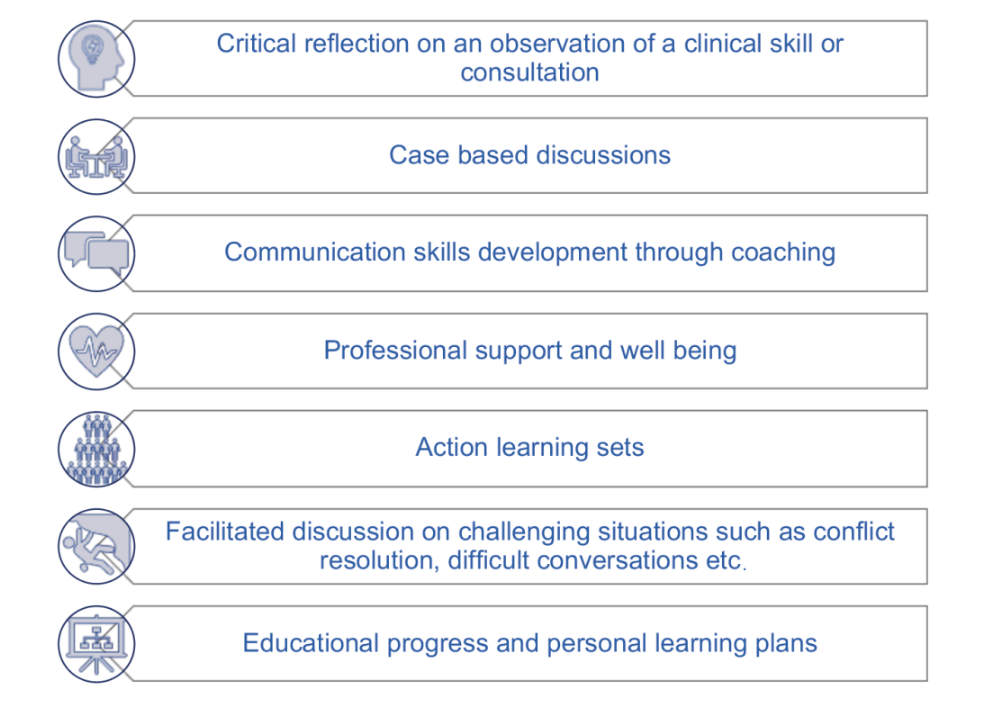
Supervision can take many forms. The diagram below illustrates just some of the different types of supervision a trainee could receive to support their development.
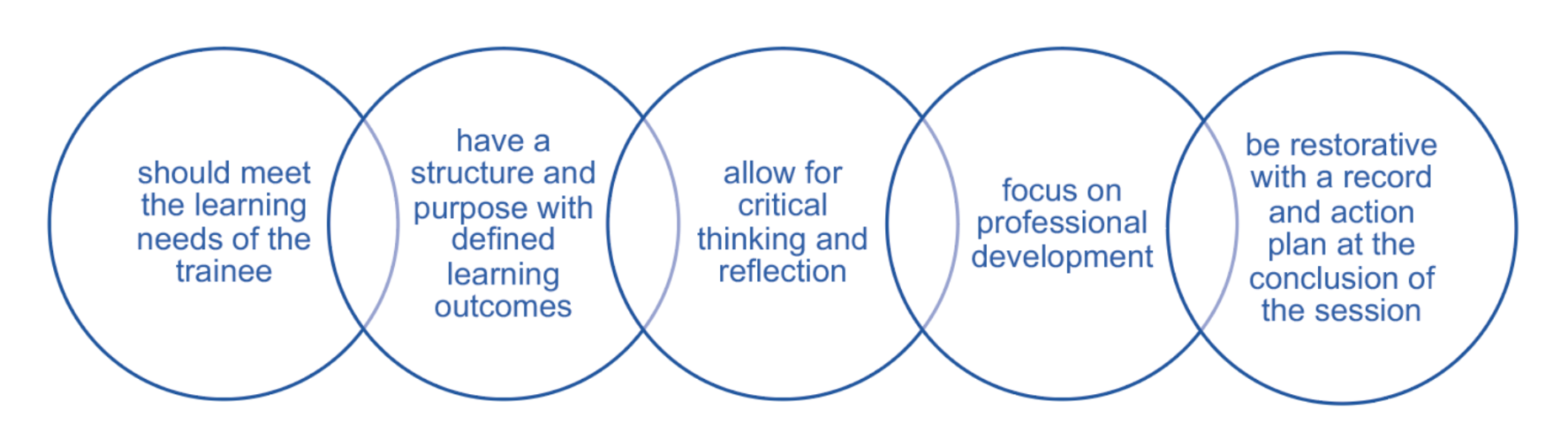
The five key elements of a supervision session
Non-urgent advice: Minimum standards:
The following must be agreed/discussed at the first meeting with the identified co-ordinating education supervisor:
- the advanced practice curriculum/scope of advanced practice capabilities which is required for the trainee role;
- an individual learning needs analysis against the relevant curriculum/capabilities;
- a learning plan which clearly identifies workplace development;
- a supervision learning contract to set expectations and boundaries.
A tripartite review of academic and workplace development with the co-ordinating education supervisor, trainee and the Higher Education Insititution (HEI) should occur once every 12 months at a minimum.
What are the trainee advanced practitioner roles and responsibilities in the supervisory relationship?
The success of the supervisory relationship is dependent on both the trainee and the supervisor actively engaging in the process.
Non-urgent advice: Minimum standards:
The trainee advanced practitioner should:
- be appraised of their own scope of practice and responsibilities as a registered practitioner;
- actively contribute to supervision, seek feedback and recognise own development needs;
- work in partnership with their supervisor to negotiate and agree the learning plan, to address performance or support enhanced learning opportunities;
- complete a “Readiness to become an advanced practitioner checklist” (Appendix 3.0) to help identify learning needs.
References
References and further resources for managers, supervisors and trainee advanced practitioners.
NHS England Workplace Supervision for Advanced Clinical Practice: an integrated multi-professional approach for practitioner development.
NHS England Multi-professional framework for advanced clinical practice in England
The Permeable Practitioner – ideas and resources to support health and care professionals to navigate uncertainty in everyday practice.
Martin, P., Copley, J. & Tyack, Z. (2014) Twelve tips for effective clinical supervision based on a narrative literature review and expert opinion. Medical Teacher 36:201-207.
NHS England, The Centre for Advancing Practice, Area Specfic Capabilities – Advanced Practice