Good practice guidance for enabling equitable access to clinical imaging referrals for registered healthcare professionals working in advancing practice roles
Publication date: January 2025
Guidance co-developed and jointly agreed with:



Guidance supported by:


Formal Letter
Introduction
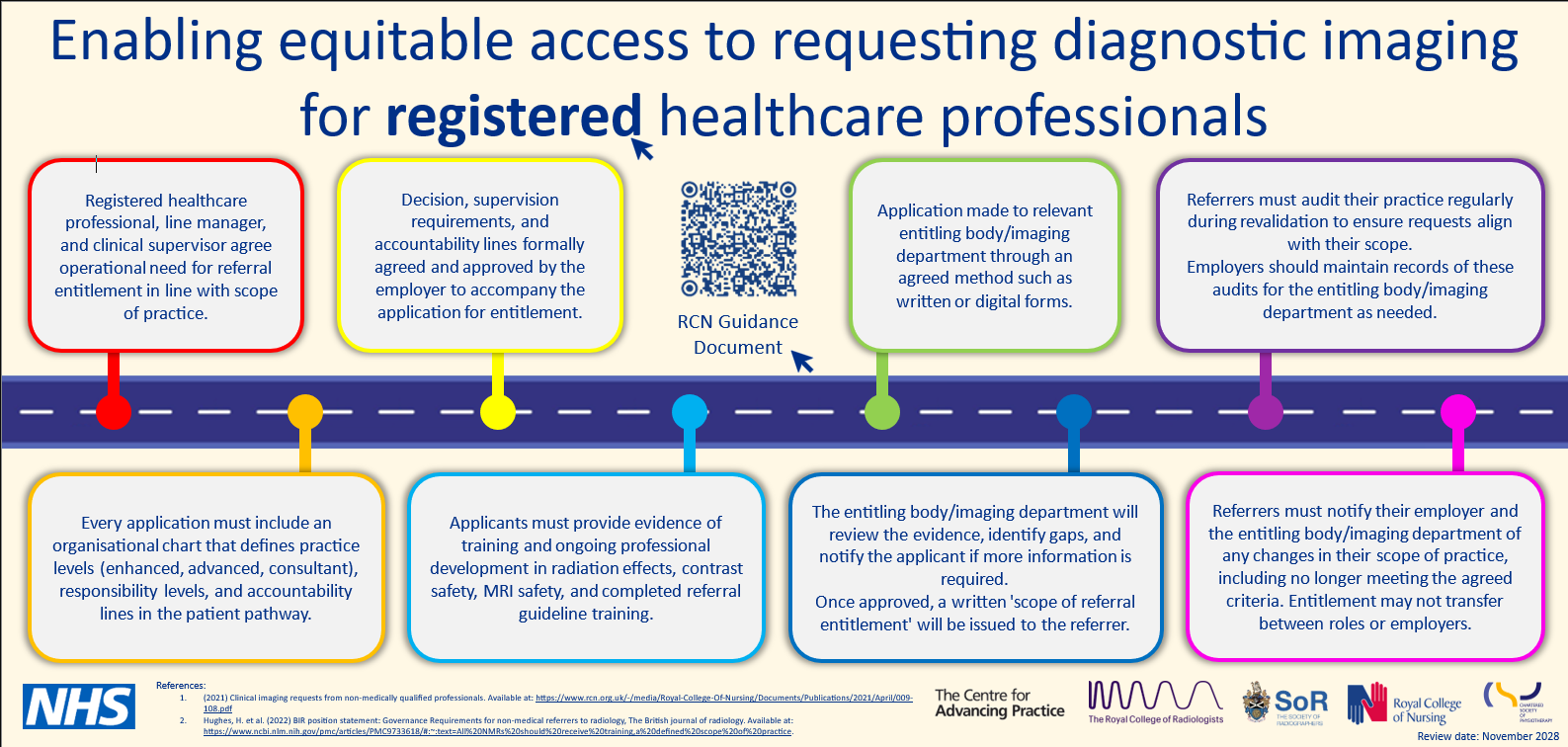
When determining access to clinical imaging requesting, inconsistencies remain across services. The 3rd edition of Clinical Imaging Requests from Non-Medically Qualified Professionals (Royal College of Nursing, 2021) recommended a standardised process.
This new jointly agreed guidance applies in all clinical settings across hospital and community care and primary care. It outlines principles for enabling more consistent and equitable access to clinical imaging referrals for registered healthcare professionals working in advancing practice roles. The guidance reminds employers and individuals across all clinical settings involved in enabling access to clinical imaging requesting of their responsibilities to support this process.
From 1 October 2024 employers are required to comply with The Ionising Radiation (Medical Exposure) (Amendment) Regulations 2024. There is a new requirement to work together where two or more employers have a shared responsibility for the referral, justification, exposure, or clinical evaluation of an individual.
Who has produced this guidance?
The guidance has been co-developed by the Royal College of Radiologists, the Society and College of Radiographers, the Royal College of Nursing, and NHS England. It is supported by the Chartered Society of Physiotherapy and the Centre for Advancing Practice.
Principles for supporting equitable access to clinical imaging requesting
- The name of the person or service to whom the employer has delegated the task of granting entitlement to individuals to act as referrers for clinical imaging should be clearly identified within the entitlement process.
- An application for referrer entitlement should contain evidence of service need and should detail the individual’s scope of advancing practice for assessing and managing patients. This should reflect nationally agreed professional standards and outline decision, supervision, and accountability lines.
- A written scope of entitlement should be provided to the referrer. This must reflect their agreed scope of practice and confirm the decision, supervision, and accountability.
- Employers should ensure that registered healthcare professionals have additional clinical imaging training relevant to their level of practice and role, such as radiation safety, contrast safety, MRI safety, and referral best practice. Employers should also specify the continuing professional development required. Nationally available learning resources such as elearning for healthcare should be used where appropriate.
- Where an individual is entitled to refer, it is their responsibility to notify the employer of any changes in their scope of practice, including when they no longer meet the criteria for entitlement. Entitlement may not be transferable between roles or employers if this is not adequately defined.
- Systems should be in place to remove entitlement for individuals who have notified the employer they no longer meet the criteria or who repeatedly fail to comply with the employer’s procedures.
- Referrers must use referral guidelines (for example, ‘iRefer’). It is the responsibility of the Ionising Radiation (Medical Exposure) Regulations (IR(ME)R) practitioner (radiographer or radiologist) to communicate effectively to the referrer when a referral is inappropriate or does not meet the referral guidelines. This applies to medical and other healthcare professional referrers. Inappropriate referrals delay the delivery of safe and effective care.
- Detailed requirements for the entitlement and identification of referrers should be included in the employer’s written procedures.
- Automated systems-based management and control measures should be developed within provider organisations and integrated care systems to ensure ongoing compliance assurance and support the management of resources.
- Referrers must audit their practice in line with professional requirements and employers’ written procedures. Where available, this could involve using the electronic patient record (EPR) to demonstrate they are requesting within their scope of practice. A record of audit outcomes should be kept by the employer.
- Entitlement to refer does not infer entitlement to make a clinical evaluation; if this is required that should be made clear at the point of application and managed through separate local appropriate processes.
Review date
November 2028 (or earlier if there are changes to the relevant legislation).
Conflicts of interest
Conflicts of interest have been considered in the development of this guidance and not determined to exist amongst any of the collaborating organisations.
Relevant guidance
The resources detailed below provide relevant information related to guidelines for employers and healthcare practitioners engaged in clinical imaging procedures, encompassing requests for various imaging modalities (both ionising and non-ionising).
Guidance on levels of advancing practice
- Health Education England: Principles of Enhanced Level Practice (2023).
- Centre for Advancing Practice, NHS England: Multi-professional framework for advanced practice in England (2025).
- Centre for Advancing Practice, NHS England: Multi-Professional consultant level practice capability and impact framework. (2023).
Guidance on requesting clinical imaging
- The Royal College of Radiologists: Implications for clinical practice in diagnostic imaging, interventional radiology and diagnostic nuclear medicine (2020).
- The Royal College of Nursing: Clinical imaging requests from non-medically qualified professionals 3rd edition (2021).
- The College of Radiographers, The Royal College of Radiologists: Quality Standard for Imaging (2022).
- The British Institute of Radiology: Guidance for non-medical referrers to radiology (2022).
Research report evaluating experiences of access to clinical imaging requesting for advanced practitioners
- The East Midlands and West Midlands: Workforce – Assessing variabilities in access to imaging requests for advanced practitioners working in acute trusts across the Midlands (2022).
Regulations for use of ionising radiation
- HM Government: The Ionising Radiation (Medical Exposure) Regulations 2017.
- Department of Health: The Ionising Radiation (Medical Exposure) Regulations (Northern Ireland) 2018.
- HM Government: The Ionising Radiation (Medical Exposure) (Amendment) Regulations 2024.