Introduction of the Multi-professional framework for advanced practice in England – Edition 2025
Who is the framework for?
The framework describes the capabilities that underpin advanced practice roles and aims to provide a consistent understanding of them. It is therefore of immediate interest to health and care professionals already working at an advanced practice level or those aspiring to do so.
It also offers guidance on implementing advanced practice that is relevant to:
- education providers developing and delivering training for the advanced practice workforce
- service providers integrating advanced practitioners to transform services
- employers recruiting, developing, and retaining advanced practitioners
- system-level leads planning workforce transformation to meet population needs
Service users, families, carers, and the general public may also be interested in understanding the role of advanced practitioners and the role they play in improving health outcomes and providing patient-centred care.
Note on national scope
This framework meets the needs of the NHS in England and does not directly apply to Wales, Scotland and Northern Ireland. As part of the refresh, we looked at the equivalent frameworks in Wales, Scotland, and Northern Ireland to ensure alignment and address any gaps (Department of Health, Social Services and Public Safety, 2016; Scottish Government, 2017, 2021a, 2021b; Department of Health, 2019; Health Education and Improvement Wales, 2023). We continue to work with colleagues involved in the development of the advanced practice workforce in the other UK countries on matters of mutual interest and to support UK-wide workforce mobility
Introduction
What is ‘advanced practice’?
Definition
The definition of advanced practice was developed and agreed by all stakeholders.
“Advanced practice is delivered by accomplished registered health and care professionals. It is a level of practice characterised by a high degree of autonomy and designated responsibility for complex decision making. This is underpinned by a post-registration master’s level award or equivalent undertaken by an experienced practitioner that encompasses all four pillars of clinical practice, leadership and management, education, and research.
Advanced practice embodies the ability to manage care in partnership with individuals, families, and carers. It includes the analysis and synthesis of complex problems, and management of clinical risk and uncertainty across a range of settings, enabling innovative solutions to expedite access to care, optimise people’s experiences, and improve outcomes”
The impact of advanced practice roles
There is a clear need for highly experienced registered health and care professionals trained at an advanced level of practice. This progression is not about creating a generic health and care professional. Instead, each clinician’s discrete professional identity as a registered health and care professional is of fundamental importance for enabling their subsequent practice as an advanced practitioner in their particular scope of practice and in a variety of settings and professional contexts.
Where optimally trained and deployed, advanced practitioners can support the transformation of services and care pathways to better meet the needs of people, their families, and carers. They can increase capability within health and care teams, by enabling the skills of individual multi-professional team members to best effect and drive improvements in population health.
What does “post-registration master’s level award or the equivalent” mean?
The phrase ‘post-registration master’s level award or equivalent’ in the definition above recognises that existing practitioners may have followed a variety of different routes into advanced practice.
Preparation for advanced practice will most often be through a master’s degree. However, equivalence at master’s level can also be demonstrated through a combination of formalised experiential learning, supported by evidence mapping the individual’s capabilities to the 4 pillars of advanced practice.
Development towards becoming an advanced practitioner is a post-registration activity that requires individuals to first gain experience of the newly qualified, foundation, or preceptorship stages of entry-level practice. This foundational experience provides the necessary grounding before registrants progress to advanced practice training programmes.
The Centre for Advancing Practice only accredits advanced practice programmes that lead to the award of a full post-registration master’s qualification and that demonstrate they meet required standards, including mapping to the framework.
The Centre’s ePortfolio (supported) route allows existing, experienced advanced practitioners who do not hold an accredited master’s qualification to demonstrate their equivalent experiential and educational learning against the capabilities.
Which registered health and care professionals are covered?
There are 9 statutory regulators of health and care professionals in England overseen by the Professional Standards Authority for Healthcare and Social Care (PSA). Some other professions are not regulated by law, but registered by ‘accredited registers’ also overseen by the PSA.
The advanced practice development activities of the Centre for Advancing Practice and the regional faculties focus on the statutory regulated professions and the delivery of NHS-funded and other publicly funded services.
The activity covered by the framework does not relate to all groups that come under statutory regulation (for example, pharmacy technicians, and nursing associates and other associate professions).
While regional requirements will vary, funding for trainees on advanced practice programmes is normally limited to individuals who:
- are registered with the appropriate statutory regulator
- have employer support for undertaking advanced practice training
- have a funded, identified advanced-level position at completion of their training
We are committed to exploring whether other professions on PSA-accredited registers – which are not currently subject to statutory regulation – require access to advanced practice education, training and development.
The 4 pillars of advanced practice
All health and care professionals working at the advanced practice level are expected to have developed the knowledge, understanding and skills required to meet all the capabilities outlined in this framework.
These capabilities define a consistent standard of practice across professions, roles and settings, ensuring uniformity and fostering confidence in the development and deployment of the advanced practice workforce.
The expected capabilities are organised under 4 pillars:
- Clinical practice
- Leadership and management
- Education
- Research
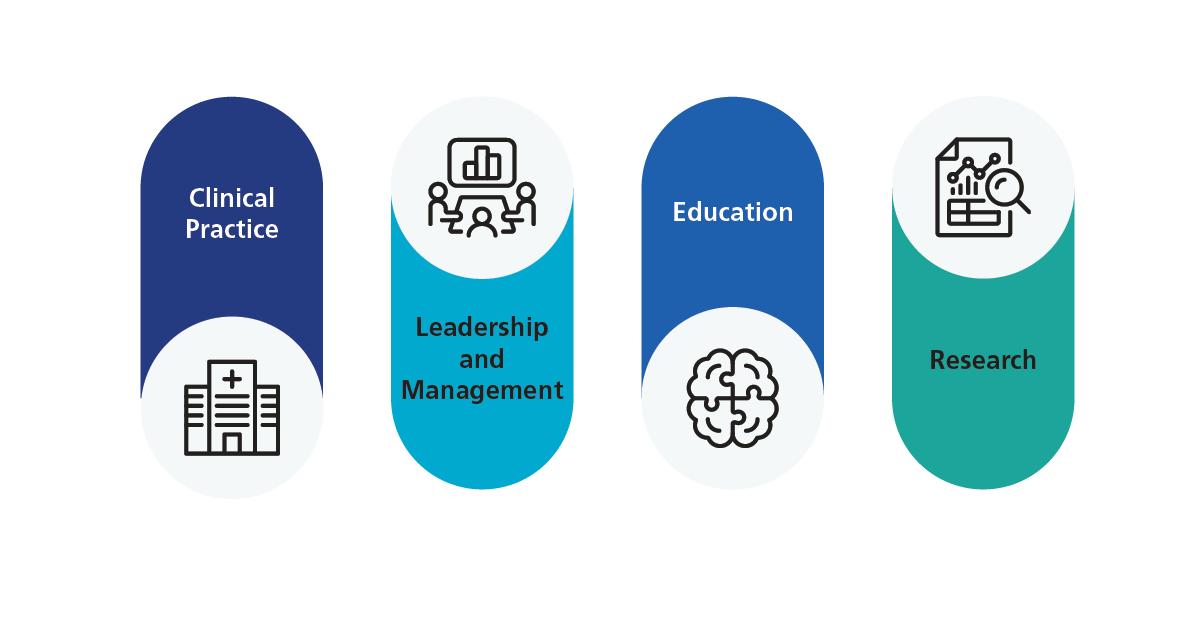
These pillars form the basis of advanced practice education, learning and practice. The language used in the capabilities is deliberately mapped to level 7 taxonomy. This refers to the academic and professional level associated with postgraduate or master’s level qualifications in the UK and some other countries that align with the Framework for Higher Education Qualifications (FHEQ) or similar frameworks. It defines the complexity, knowledge, and skills expected of learners. This supports and makes clear the expectation that health and care professionals working at this level practice at master’s degree level.
That expectation means advanced practitioners should have the ability and experience to make sound judgements in the absence of full information and to manage high levels of risk, including in the context of complex, competing or ambiguous information or uncertainty.
The developmental pathway toward achieving advanced level practice will be different for individual practitioners. Health and care professionals will demonstrate these capabilities in different ways, tailored to the scope, context, role, and profession in which they practice.
We have provided further information below about how the capabilities outlined in the Framework relate to medicines and prescribing, environmental sustainability and equality, diversity and inclusion.
Medicines and prescribing
The capabilities refer to advanced practitioners being able to: “Initiate, evaluate and modify a range of interventions which may include prescribing medicines, therapies, lifestyle advice and care.” (see 1.7).
Legislation sets out the specific regulated professions that can access mechanisms to administer, supply and prescribe medicines. Not all regulated professions can currently access these mechanisms, but legislation may change over time.
The ability to prescribe does not define advanced level practice. The capabilities do not specifically require health and care professionals to be able to prescribe or access other medicines management mechanisms to practice at an advanced level. The ability to prescribe may be an employer requirement for some advanced practice roles, for other roles it will not be a requirement.
Environmental sustainability
With all 4 UK health services committing to net zero, every health and care professional must take action to deliver high quality, low carbon care that addresses the health, care and wellbeing needs of individuals, families and carers – both now and in the future.
Sustainable health and care must be underpinned by strong clinical leadership, with its principles embedded into governance structures and policies. Then enhacing it’s effectiveness through workforce training and development. Advanced practitioners, as leaders within teams, organisations, and systems, are strongly positioned to transform the design, development, and delivery of clinical care and services, with their leadership playing a pivotal role in achieving sustainable healthcare.
The capabilities outline below reflect this responsibility and stipulate that advanced practitioners must:
- act as role models and advocates for developing and delivering care that is responsive to changing requirements (see 1.10)
- continually develop their practice in response to the changing needs of the population (see 2.9)
Equality, diversity, and inclusion
Advanced practitioners have a crucial role to play in eliminating discrimination and promoting equality, diversity, and inclusion. We have an individual and collective responsibility to ensure that all health and care provision meets the needs of the diverse population, regardless of background.
The NHS equality, diversity, and inclusion (EDI) improvement plan sets out actions to promote fairness, eliminate discrimination, and foster inclusive environments for patients, staff, and communities across the NHS. This includes, but is not limited to, those with protected characteristics under the Equality Act 2010:
- age
- disability
- gender reassignment
- marriage and civil partnership
- pregnancy and maternity
- race
- religion or belief
- sex or gender
- sexual orientation









The capabilities outlined in this framework highlight the importance of inclusive, person-centred care that is focused on the needs of individuals. To strengthen this focus, capability 2.1 of the leadership and management pillar has been updated in the refreshed framework so that it puts more emphasis on inclusion.
We are committed to providing all practitioners with equal opportunities to move into advanced practice roles. The framework supports employers and education providers in training and developing advanced practitioners and is designed to ensure these development opportunities are accessible to regulated practitioners across different specialties, sectors, and settings, while helping the NHS align workforce development and deployment with population and service needs.